For a more detailed exploration of this topic be sure to check out the Wikipedia article on Grinding Teeth and Tooth Wear – or Bruxism.
For more about how to CONTROL your stress and anxiety and how it impacts your jaw – you should learn about the Feldenkrais method of awareness through movement – specifically as to how it involves the jaw.
Organization of this Chapter
You May Skip to Whatever Subject Interests You Now
Basics
The Nature of the Problem
Detection of Wear
Causes of Grinding
Treatment Options
Bottom line for Grinding
…………………………………………………………………………………………………………………………
Basics
In order to get a feeling for the esthetic consequences of grinding teeth, look at the pictures below. The first picture shows the smile (with the lips pulled back out of sight) of a person who has ground the anterior teeth flat, and even shortened the teeth considerably in the process. This is compared with the smile of a person who has teeth of normal length and contour. These two people could be the same age and general appearance, but the shapes of the teeth would make the first person look considerably older. Why is this? Older people tend to have flatter teeth, so in the back of all of our minds is the thought that flat teeth equates to advanced age.



The third photograph shows more of the posterior teeth as they may get after a lot of grinding. Here again, the flat teeth make the person look old, but also chewing has potentially become a problem as well. Excessive wear on the posterior teeth can lead to many difficulties, though there are some people who have everything ground quite flat who seem to have adjusted quite well.
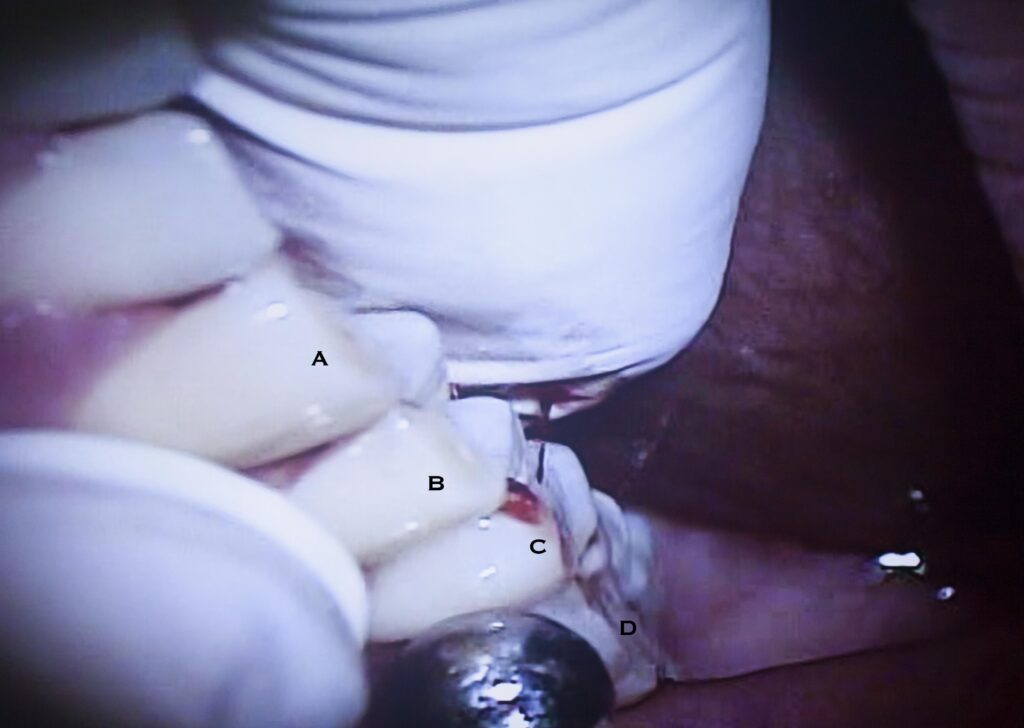
The person in the picture below shows a canine, labelled “A” which is very flat, and the outside cusp of the first premolar “B” is just as flat. You might even see a little circle in the middle of each where the dentin is exposed and wearing faster than the enamel. For the most posterior teeth, “C” and “D”, clearly the cusps have been flattened too.
When I see an 18 year old with flat teeth it makes me worry. Here’s someone who has at least 60 years more use to get out of these teeth, and yet they’re half gone already, after being in the mouth for only 6 to 12 years! What can we do about this? What causes this kind of damage? We’ll look at some of these concerns in this chapter.
Tooth wear is one of the THREE BIG PROBLEMS with teeth. It seems that everyone has one of the big 3: decay, periodontitis or wear. Out of a thousand patients I’d feel lucky to have one (and I have) that at an advanced age has no history of more than slight decay, no periodontal pocketing, and no sign of wear. The bad news is that for every person that you can tell “you’ve got no cavities” to, you have some bad news anyway. Either their teeth are in jeopardy due to gum disease, or because they’re grinding them into little flat stumps, or the pressure is causing other problems (visit Chapter III.5). Can you imagine my dismay with the 18 year old above to have to say that unless some preventive measures are taken, within 10 or so years all the teeth will have to be crowned!
The Nature of the Problem
From the introductory paragraphs and pictures you must have a pretty good idea of the appearance of excessive wear. But we really have to decide what NORMAL wear is as a starting point. By the age of 50 most people have started to show some wear on their canines. For women at this age, the upper incisors normally won’t be flattened, but for men they often are. One theory is that the stress of the workplace has caused men to take out more tension and aggravation on their teeth. OK – these days it’s a pretty huge and often incorrect assumption that men are more involved in a stressful workplace than women! Maybe its some combination of this and the likelihood that men’s jaws exert more force on opposing teeth in response to stress than typical for a woman. At the very least it must also be said that household stress with a couple of teenagers should be as difficult as workplace stress. Even with most women of today in the workforce for those that stay home things might be expected to even out. I suspect, however, that there is some more fundamental component to the makeup of men versus women that causes a difference in the propensity to grind their teeth.
But if we assume that slight to moderate wear is normal for the 50 year old, we must note that there are many people with severe wear at a far earlier age, and to reach an older age with little sign of wear is almost unheard of.

It isn’t just permanent teeth that are affected by wear. Every once in a while you see a young child of 6 – 8 whose baby teeth (primary teeth) are ground out so each looks like a little cup, instead of a tooth. The good news is that decay is more unusual in these cases, the grinding moves faster than the decay and removes the susceptible grooves of the tooth. The other good news is that, most often, when the permanent teeth come in the grinding will not continue at that rate. It is poignant to note that kids that do this often have just gone through their parents divorce, one parents death, or another major family tragedy. It may SEEM that kids fail to notice things, but their teeth may tell a different story!
We’ll talk more about the cause of abnormal wear later, but at this point it must be indicated that most of it is not due to chewing. There are exceptions – people in villages where dietary flours and meals (corn meal especially) are ground in stone mortars often have very flat teeth due to the amount of stone in their food. Also, some tribal communities in the world indulge in rituals or social patterns that lead to wear. But most of the time the wear is directly caused by PARAFUNCTION. Parafunction is, as the name would imply if you were Greek, counter to normal function. Normal function where the teeth touch would consist of swallowing and to some extent chewing, depending on the food. But parafunction is where, for some reason, the person elects to bring their teeth into occlusal contact and then grind them around for 6 to 8 hours.
Most of the time, when an abnormal wear pattern is detected, the grinding takes place at night. The name given to this activity is NOCTURNAL BRUXISM. The person is rarely aware of doing it, but the spouse often is! Can you imagine sleeping with someone scraping their fingernails on a blackboard all night? OK – not the same with the more commonplace whiteboards these days – but you get the idea if you are of a certain age. Most of the time the sound isn’t that bad, but the informed person will find it to be a scary sound. Consider the need for a $25000 mouth rehabilitation after 25 years of grinding. One thousand dollars per year translates into how much per grind?
The worst cases of grinding also work on their teeth during the day, and are frequently aware of doing this. The pattern typically is that after an intense period of concentration there is a sudden awareness of very tired and sore muscles in the cheeks. They are sore because they were working so hard, when the person didn’t even know it! Sitting on a stopped freeway is often a likely culprit!
Other kinds of habits can lead to wear. Chewing straight pins or bobby pins can often lead to notching of favorite teeth at the incisal edge. I once had a patient chat chewed nails for 35 years as a carpenter. He said the wear was due to the nails, but the teeth fit together so well, it was obvious they had been ground flat against each other.
Detection of Wear
The qualitative estimate of wear can often be made in an instant by the dentist or informed person. Just look at the incisal edges of the upper canines and incisors of an individual. If they are flat then you know that the person is engaging in some sort of parafunction. As we’ve discussed above, even the untrained observer can get an impression of someone’s age by unconscious evaluation of the flatness of these teeth.
The QUANTITATIVE determination of wear is much more difficult, however. Anyway, would the dentist want to evaluate wear in a precise fashion? More than likely it would be part of a research project, where for example the abrasivity of some material, or the resistance to wear of another material is being measured. But there are certainly situations where one would like to track the amount of wear on a patient’s teeth with precision, such as could give some predictability of the short and long term consequences of wear patterns.
The way in which the dentist can record wear areas is by taking an impression and making a model (correctly called a cast) in some material. This permanent record for a particular time can be measured using rulers or even scanning, computer-driven microscopes. What is being measured? For each tooth we look at the size of the wear facet – like the facets cut onto a gemstone – it is a flat spot ground onto an otherwise curved surface. For the posterior teeth wear facets will appear on the inclines of various cusps, depending upon which areas are in parafunctional occlusion with opposing cusps. For the anterior teeth the wear facets are right on the cusp tips (canines) or incisal edges. For the incisors a measurement of facet area is probably less important than an estimate of lost length (made with an assumed initial length, or by sequential measurements made over the years).
Note again, that evidence of wear is normal. It is not nominal, however. Normal wear, though, will not result in the need to restore the teeth by the age of 50. It is the progression of abnormal wear that we are keenly interested in measuring.
If you think that you have a wear problem, have your dentist take impressions so that a record may be kept. Few dentists will have the facilities to measure the casts accurately, but if a severe problem seems to be showing up, then he can consult with a nearby dental school and have adequate documentation to make some informed decisions. A severe problem is one that can be detected easily by eye on casts that were taken just a couple of years apart.
While wear is the most common manifestation of grinding, another observation that is sometimes made is that certain teeth become MOBILE that are otherwise not affected by periodontal disease. Often one or two incisors are set so that they take the load of a parafunctional action. These teeth will have such stress applied to them that the bone that supports them will resorb away from the root. This is not necessarily a permanent bone loss, as in the periodontal disease situation, but the involved teeth can become very loose. Often in these circumstances, it is best to shorten these teeth slightly so they don’t hit any more than the neighboring teeth, and then stabilize them while the bone in the socket reforms to the stationary tooth.
The situation described above is much like the case when a person wears braces. Exerting a force on teeth causes the bone to resorb and allows movement. If a person in active treatment with braces were suddenly to have them taken off, before allowing the teeth to stabilize, you would be amazed how loose the teeth would be!
Causes of Grinding
Here’s where we get into a real fight. It’s the same fight we will get into later when discussing disorders of the TMJ (visit Chapter III.6), and when explaining the non-carious (no decay) cervical lesion – Chapter III.5. The problem is that no one really knows what is going on with dental wear, but most people have an opinion!
Obviously, abnormal wear is caused by parafunctioin in almost all cases. But what causes the parafunction? As has been alluded to before, it is clear that emotional stress has something to do with it. But why do certain people take stress out on their teeth? Again, speculation runs wild. We know that many people that get ulcers are stress-prone individuals. But do all highly stressed people get ulcers? Nope. So, maybe it is an abnormal stomach combined with the stress that does the trick. Abnormal stomach could be one that secretes more acid as a consequence of stress than is normal, or one whose lining is less resistant to acid than normal.
It is speculated, not proven, that a person whose teeth don’t fit together well has a tendency toward parafunction. If you slide your teeth around and discover some place where the teeth don’t move smoothly over each other, you have an eccentric interference. Now – the teeth are DESIGNED to have an eccentric interference with the canine guidance we’ve discussed in Chapter II.5. So perhaps the body expects that. If you are a nervous, stressed individual, you might try to remove that interference by grinding your teeth together. It seems to be human nature that we tend to attempt to eliminate any body abnormalities even if it causes great pain and discomfort. How many people can get a pimple and simply leave it alone? If you find a dry, crinkly hair growing out of your head, do you just leave it there? When the dentist places a filling or a crown in your mouth that feels high (it hits when its neighbors don’t), most people keep “testing” it, over and over, tapping and rubbing and squeezing until the tooth gets very sore. Perhaps a smaller discrepancy stimulates tapping and rubbing, not so much as to make the tooth sore in an acute sense, but can lead to a chronic, long-term problem: wear.
It is known, from some very imaginative research, that an occlusal discrepancy of as little as 7 microns (.007 mm) will alter the muscle patterns in the swallowing reflex. The average hair diameter is 50 microns! Such a small defect can then have a subtle effect on function, and could, in principle, generate an unconscious parafunctional habit. No relationship between the magnitude of response to the stimulus and the general stress level of the individual was investigated.
Ideally, the research would have been done that shows the relationship between emotional stress, occlusal discrepancy and tendency toward parafunction. If there were then a written exam from which one could extract a meaningful indicator of stress level, and one could measure occlusal discrepancy with sufficient precision, one could hope to predict which patients could have a parafunctional problem. The barriers to the completion of the research are that the determination of emotional stress is not that easy, and that measurement of the precise nature of a person’s occlusion with such precision isn’t possible. The factors that control whether a person has the tendency toward taking stress out on the teeth or not is likely to remain elusive.
So we really can’t prove at this point that the occlusal scheme initiates the release of psychological stress on the teeth. It is still, however, a pretty good guess and a good working hypothesis until methods come along which permit an appropriate study to be done.
Now I will share with you a personal experience. I am an anxious person by nature – and am very driven to get things done. When things don’t get done efficiently and well it upsets me. Then I tend NOT to slow down and take a break, but charge ahead with more vigor until I bulldoze my way to a successful conclusion. But it takes a toll on me.
I am learning to recognize how anxiety shows up in my body – often by a TAPPING of my teeth together, rapidly – tap, tap, tap – mostly toward the front of the mouth. This is a hugely habitual behavior, which I think goes back about 10 years to my divorce.
If I can learn to recognize this habit – sense at all times when I am tapping my teeth, I’ll know when I am anxious, and can take steps to slow down. One motivation to slowing down, is that I become a person more pleasant to be with.
Tracking the awareness of the tapping is my goal now. How does one learn to be more AWARE of their jaw behaviors? There are ways to become more aware of yourself through awareness of movement – and the principle modality of this is the Feldenkrais Method for Awareness Through Movement. The link above will show you a series of audio recordings that will direct you to more awareness in your jaw.
I do these movement lessons every day with the goal of expanding my awareness of anxiety more and more. There are many Feldenkrais lessons, enabling awareness of all parts of the body, that may be indicators to you of your stressful and anxious state.
Treatment Options
There are really two aspects of treatment that must be considered. There is the repair of the damage caused to date, and there is the prevention of further damage.
Restoration
Restoration of the damaged areas will have different strategies depending upon the number of teeth involved, extent of destruction and whether the teeth will be protected in the future. It may be that a person has flat incisors and wants them fixed. If they are built up with plastic material to look like they did originally, then it won’t take too long to knock this material off once the subconscious lust for destruction takes over. If the canines have wear facets, and this is what allowed the incisor interference and led ultimately to the flatness, then as long as the canines are restored, then the incisors will be protected. Is it possible to restore the canines with enough strength to again provide their original protective function? In moderate cases of bruxism it is.
Even in the case where both incisor and posterior wear is moderate, restoration of canines can help to have a preventive function, because when you slide your jaw sideways or forward, the canines on the top and bottom force the jaw to open, and the other anterior teeth and posterior teeth to separate, or disclude. But it is advisable to reduce the chances for further nighttime damage by also providing the patient with a nightguard.

A nightguard can take many forms, but basically it is a soft and flexible appliance that is worn over the (usually) upper teeth at night. It generally can be worn with no discomfort and is quite effective in protecting the teeth from grinding. It also protects the ears of your sleeping partner!
It may be that changing the entire occlusal surface with a guard takes away the stimulus to grind. Patients don’t tend to chew these things up, and they don’t tend to look, even after extensive use, like they are subjected to as much abuse as the teeth were.
On the other hand, I remember after I had my braces taken off I was given this large black rubber thing that I bit into and was supposed to wear at night. I can still taste it in my mind! This positioner was not a nightguard but an orthodontic retainer, or sorts. One dream I particularly remember was of myself eating a very, very tough steak. That was a $100 dream and the last of my positioner.
Restoration of the teeth when the posteriors are worn flat can range from doing nothing to doing everything. Some of my patients are absolutely flat sliders, the teeth have no points at all, and the lower teeth can assume any position relative to the upper ones in contact. The occlusion isn’t really “flat” in the geometric sense of the term, it could be considered an undulating, twisting plane when moving from a molar on one side to the other. But, if the loss of tooth structure is not too severe, many patients seem to do fine in this condition. Eating that steak (a real one) can be difficult with the best of cuts, but they manage. Forms of damage that a flat occlusion and concomitant sideways grinding chewing pattern can have is to the outside surfaces of the teeth, the boney support and the joints.
We will take a look at damage to the outside, facial, surfaces of the teeth in Chapter III.5. It, in many cases, is thought to be due to tooth flexion in situations of laterally imposed stress. Such stress would be maximized when the teeth are not completely flat, but where there is still a lateral interference. Nonetheless, there can still be some flexion with a flat occlusion, depending upon the amount of force exerted.
If there are not many teeth to take the load of parafunctional grinding or chewing by lateral grinding on flat teeth, then it is possible to make these posterior teeth mobile. This is a traumatic mobility. It is not clear whether this can lead to a permanent loss of supporting bone, but over the years may exacerbate a tendency toward periodontal disease, and this would cause permanent loss of support.
The joints were not designed to support a cow-like chewing pattern. Again, it may be symptomless, but considerable damage to the disc of the jaw joint (temporomandibular joint, TMJ) can happen due to extreme stress associated with an inefficient chewing function. The stress on the teeth that caused the loss of occlusal anatomy will be transmitted to the joints and can cause damage. When we talk about the joints in more detail (visit Chapter III.6), we will cover the nature of preventive and restorative possibilities (see also Chapter V.17). Let it be said that if all of the teeth are rebuilt to their original shapes, fitting together well and providing good chewing efficiency, then further damage to the teeth is prevented, but the restored surfaces are generally not subject to the kinds of stresses that originally damaged the teeth. Also, the pressure on the joint can be relieved, stabilizing their condition.
In the case where the tooth wear is so severe that there is little tooth left, either in the anterior or posterior segments, full restoration must be done. Generally, this entails having artificial crowns cemented to every tooth, rebuilding their original anatomy and height. All of a sudden the chin and nose will be as far apart when biting down as they were originally, and this will have a dramatic effect on the appearance. But most importantly, the cycle of continuing damage can be effectively arrested, and this includes damage to the teeth, bone and joints.
Generally, this full mouth rehabilitation is done only when the patient reaches a point where further loss can have dire consequences. To some extent this is due to the high cost, complexity, and difficulty of the procedure when done with all deserved rigor. But it is also due to the fact that many patients just don’t develop symptoms. The teeth, even though lots of dentin is exposed, are not particularly sensitive. This is due to the filling up of the dentin tubules when the grinding takes place over a large period of time, and pulpal recession. But, eventually the teeth will be worn so far that the smile becomes very unattractive, and there isn’t really enough left on which to place an artificial crown. Then a root canal procedure will have to done on every tooth in the mouth before the crowns can be placed! Isn’t that an exciting prospect!
Prevention
As was mentioned above – a nightguard may be of some help in preventing wear – especially if worn at night. But, it will not typically be worn all the time, and cover the time when most damage is done for a particular person.
On the other hand – the best solution is to become AWARE of the grinding, and the stress and anxiety that underlies it. I mentioned above the Feldenkrais Method, whereby you might become more aware – but there are other modalities where awareness may become possible.
I am no psychologist, to be certain, but have visited several on occasion. The goal is to become aware of stress and anxiety on a moment-to-moment basis throughout the day – and anything that helps to achieve this is helpful. Talk therapy is not likely to be of help, unless you take suggestions home and put them to use on a daily basis, or an hourly basis, or constantly throughout the day.
Bottom Line for Grinding Teeth
We’ve seen how grinding habits can be stimulated by emotional stress and an imperfect occlusion, and how they can result in significant negative alterations of the appearance and total destruction of the teeth and often of the joints. Correction can range from restoration of a few areas and then provision of appliances preventing further grinding damage, to complete rehabilitation of the mouth, often running over $50,000.
It must be emphaized that there is no widely accepted proof that occlusal interferences stimulate grinding, or that the stress of grinding will damage the joints. But these are good working hypothesis, and the dentists who specialize in oral rehabilitation find, in the great majority of cases, that the treatment will stabilize the mouth to further damage by grinding and that even damaged, symptomatic joints can be stabilized when the bite is restored in the correct jaw position.
The subject of bite irregularities continues in the next two chapters. In the next (Chapter III.5) we will consider the causes and restoration of the wedge-shaped notches on the facial surfaces of many people teeth. While often attributed to incorrect toothbrushing, the cause is more likely to be faulty occlusion and stress, the same things that can stimulate grinding. In the chapter after that (Chapter III.6) we will discuss joint problems and facial pain syndromes, each of which may have a relationship to the bite and to stress as well.
So, we’re really establishing a thought that stress and poor bite in combination MAY well result in a variety of damage, requiring three chapters to discuss thoroughly. This makes occlusion a kind of focal point in several very common and severe types of oral disease, and yet the vast majority of dentists and the dental community as a whole don’t really understand the subject. Many suspected cause-and-effect relationships have not been proven and those who spend the time to learn what has been done in the field often find that their conclusions differ from those of others who have also studied the situation carefully. This field can make good use of the finest minds available, and the last word has not yet been said.
And this is true as well of what interceptive measures may be helpful for any particular individual. Being aware of, and controlling stress and anxiety is certainly a great place to start!