If you would like to explore more around the subject of tooth pulp infection, also known as pulpitis, you may connect to this page of Wikipedia.
Organization of This Chapter
You May Skip to Whatever Subject Interests You Now
Basics
Pulpal Recession
Approaching the Pulp and Symptoms
Exposure of the Pulp Chamber
Continuing the Bacterial Invasion
Bottom Line for Infection: Pulp
………………………………………………………………………………………………………………………….
Basics
As the tooth decays, whether it is through the occlusal, biting, surface of the tooth, invading through the grooves and pits, or from the surface of the tooth which abuts the adjacent teeth, or from the surface of the exposed root after gingival recession, when this decay goes on long enough it passes through the enamel, and potentially through the dentin and possibly exposes the pulp.
When the pulp has been exposed by the decay process, the bacteria which produce the acid which erodes the tooth structures, find a new place to live – the pulp chamber.
Pulpal Recession
Now – the teeth are designed to prevent the exposure of the pulp – by forming more dentin inside the pulp chamber near the site of close approach – in essence the pulp chamber is running away from the advancing army of bacteria. BUT – if the advance is fast, more rapid than the odontoblasts (visit Chapter II.2) can wall off, then a frank exposure happens. If the advance is slower, then the pulp recedes into the tooth just ahead of the eroding dentin, maintain a thin but insulating wall of newly formed dentin between.
As the dentist removes the decayed tooth structure he/she will be very careful the farther into the tooth they go, because it may not be clear just how close to the pulp the decay has progressed. There may only be a .5 mm layer of healthy dentin between where the dentist is working, and the pulp chamber.
Approaching the Pulp and Symptoms
Picture if you will, as more and more of the decayed tooth structure is cleaned out, passing from a very soft and gel-like substance, to a kind of leathery dentin, (in which the bacterial have not leached out all of the mineral content), to a harder dentin which can still be scraped away with an instrument, to healthy dentin that is resistant to scraping away. Ideally, by the time the dentist has removed the decay totally, there is still a thin layer of hard dentin left covering the pulp chamber. This dentin has not been demineralized at all, and does not contain any of the decay-causing bacteria. It may even be possible to see the red color of the pulpal tissue THROUGH the thin layer of dentin – and this tells the dentist they are close to an exposure, AND that there is still blood flow into the pulp.
You may think that the patient, you, might have experienced pain at this point when the decay has advanced so far. You may be right, but not always is pain associated with this invasion. And, if it is, it is not “toothache” type, throbbing pain. The pulp is working quite diligently to wall off the decay, but there may be some acid from the bacteria that have leeched through the otherwise solid dentin to the pulp chamber, to the extent that the pulp is irritated. This pulpal irritation may result in what we call HYPEREMIA of the pulp – it is a kind of excessive response that may make the pulp more sensitive, particularly to cold temperatures in the mouth.
Another condition that may develop as the pulp is approached closely by the decay process is REVERSIBLE PULPITIS. This is a pain that results from the inflammation of the pulp – recall that any word ending in “itis” is referring to inflammation of something. In this case the reversibility can be demonstrated by the fact that the pain which is experienced with cold temperatures, biting down on the tooth, or even hot temperatures is NOT long lasting. There is no pain of DURATION. In other words, it hurts for a few seconds, no more than 30 seconds, and then it feels OK again.
Later (visit Chapter V.2) we will discuss procedures associated with the restoration of this deep decay when it does NOT expose the pulp. But for now we need to look at what happens if it DOES expose the pulp.
Exposure of the Pulp Chamber
Picture again the removal process of the variously degraded dentin as the dentist works farther and farther into the substance of the tooth. It is quite possible that when the dentist reaches the point where the dentin is leathery and easily scraped away, some bleeding starts in the deepest area. In this instance, it is clear that there are bacteria in the pulp chamber, because the penetration of the bacterial is considerably beyond the point where it has made the dentin leathery. The bleeding is from the pulp chamber, the this exposure of the pulp likely leads to tooth pulp infection.

There WILL be more severe symptoms associated with this condition, as long as the pulp cells are still alive. Particularly, there will be pain of DURATION, indicative of IRREVERSIBLE PULPITIS. The pulp is inflamed so much that the nerves are extremely sensitive to everything. In fact, this is why the “root canal” therapy has gotten such bad press. If the tooth has been aching and there is pain of duration, the pulp is severely inflamed and invaded by acid-producing bacteria. The acidity of the pulp has increased, and when the dentist attempts to NUMB the tooth by injecting anesthetic, the anesthetic works more slowly into acidic areas, and it is much more difficult and time-consuming to patiently numb the area.
When there is pain of duration and a frank exposure of the pulp that the dentist discovers when excavating the decayed tooth structure, it is clear that the entire pulp chamber and canals will have to be cleared out of all organic, living material.
Once exposed and contaminated by bacteria, there is very little chance that the pulp will be able to recover from the insult. A lot of this fragility has to do with the fact that the blood flow into the area is necessarily poor, being only from the root apices.
Continuing the Bacterial Invasion
Once the bacterial infection has established a “foot-hold” in the pulp chamber, it can easily extend down into the canal system, and even OUT INTO THE BONE. Often, by the time the bacteria has reached the bone, the pulp tissues, including the nerves inside the pulp are dead or necrotic. Since dead nerves cannot generate sensory impulses to the brain, the tooth NO LONGER HURTS. There is no toothache as was experienced before – but the infection is continuing!
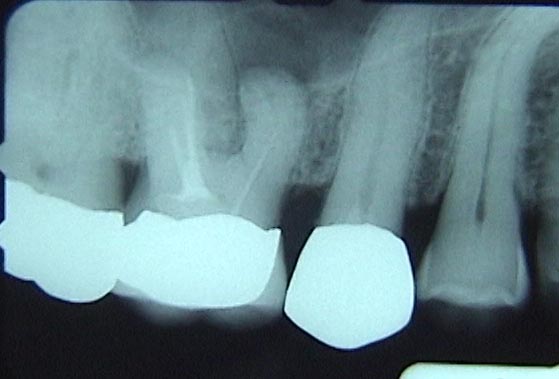
When the X-rays are checked by the dentist, one of the first things he/she will look for is evidence that there is demineralization of the bone around the area of the tooth root apices. This “periapical radiolucency” is a definite sign that the tooth has been invaded, the pulp exposed and probably necrotic, and that the infection is in the bone. AS LONG AS the dentist confirms that the darker area in the X-ray is actually located exactly at the apex, this is a firm conclusion. TWO different X-rays at different angles are required to prove that it is not some other phenomenon (like the mental foramen, shown below). In the case of a foramen (hole in the bone for nerves to pass), two different views will show the darker area in two positions relative to the apex.

When the bacterial invasion has reached the bone, the body has more access to the area with blood-born immune components, so the infection is generally limited to that area. There is acidity and inflammation in the area, however, and there are nerves in the area, so the bone might hurt when the tooth is used for chewing or hit in some way.
But the bone lesion will not resolve – the bacteria cannot be totally defeated – until the source of the bacteria is stopped. This requires the tooth to be totally cleaned out of bacteria and organic material, and filled totally with a substance that will block any additional bacterial insult. Once this is done, the infection in the bone will resolve completely, and the bone will grow back in the area of the tooth apex and the radiolucency, the dark area, of the X-ray will go away.
When the infection enters the bone, the loss of bone in the area of the apex may be because a cyst is formed at the apex, or an abscess. The ABSCESS is more serious. It is like the inflamed area around a splinter, where pus forms and eventually pushes out the splinter. In the bone the pus that forms must go somewhere and it will often find an escape route THROUGH the bone by making a small tunnel in some direction – often into the periodontal tissues or the tissues overlaying the bone. The pus is composed of dead bacteria and immune system cells that the body makes to protect your from bacterial invasion.
When the body’s immune system is not efficient enough to stop the bacterial infection in the immediate vicinity of the tooth root, the infection may migrate to other parts of the body. I have even heard of a person where the infection ended up in their BRAIN! THAT, of course, is really serious.
This just points out that when you have an infected tooth, best to get it taken care of because the body MAY not do it for you.
Bottom Line for Infection: Pulp
As the decay-causing bacteria invade the tooth, there is a fine line where the tooth can fight off the invasion and where it cannot. As long as the dentist removes the decayed tooth structure and the bacteria causing it, and fills the area to natural tooth contours, most often the pulp will remain vital and symptom free. If the dentist does not get there in time and there is significant irritation of the pulp or frank exposure, the vitality of the tooth is either questionable, doubtful, or doomed. But, the tooth can be saved IF there is not so much loss of its structure as to make restoration impossible.