For those wishing to explore dental implants and prosthetics in more detail – Wikipedia has an excellent section on this subject.
The introduction to this more detailed treatment of implants was given in the chapter on tooth replacement.
Organization of this Chapter
You May Skip to Whatever Subject Interests You Now
Introduction
Dental Implants and Prosthetics: Basics
Planning the Case
How Failures Happen
WHO does the work?
Expense!
Dental Implants and Prosthetics: The Principles
Indications and contraindications for implants;
Osseointegration
Classification of Cases:
Region of the mouth;
Nature of the bone;
Existing structures in the area
Design Concepts for Prosthesis:
Complications with bad Design
14 things which influence the design
Loading of Implants
Success/failure
Nature of forces
Mechanical models
Does reality match models?
Bottom Line for loading Issues
Placement of Implants
single tooth
multiple unit bridges
guided placement and replacement
teeth in an hour?
Home Care
Bottom Line for Dental Implants and Prosthetics
……………………………………………………………………………………………………………………….
Dental Implants and Prosthetics: Introduction
This has certainly become a popular area over the last few decades! As we’ve discussed, when replacing a missing tooth, we can anchor the replacement appliance to the adjacent natural teeth, or to one or more implants.
What is an implant?
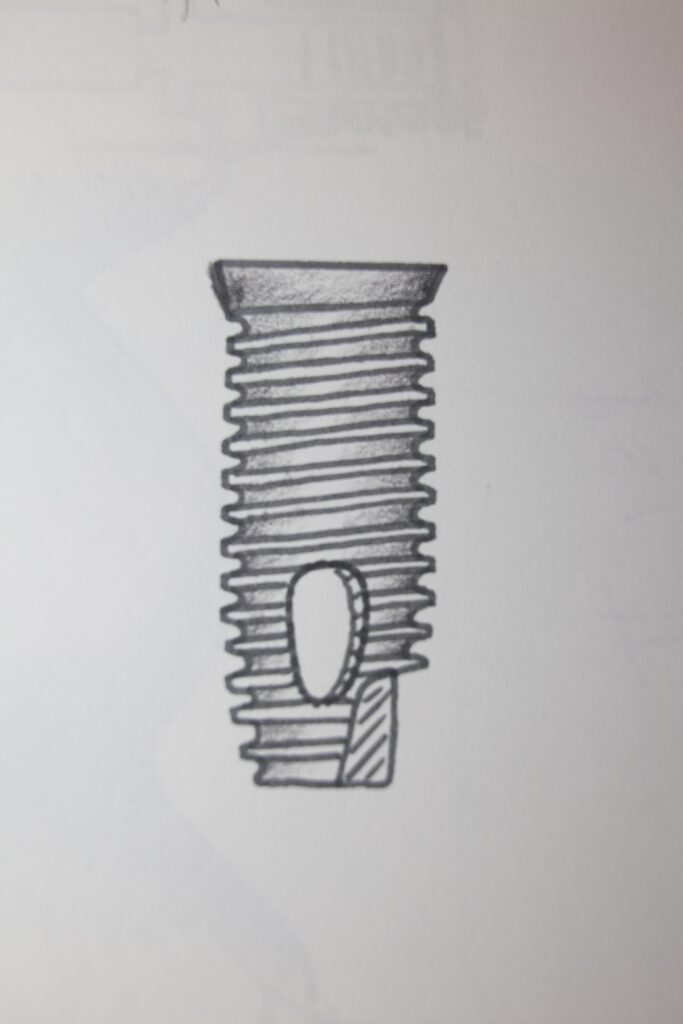
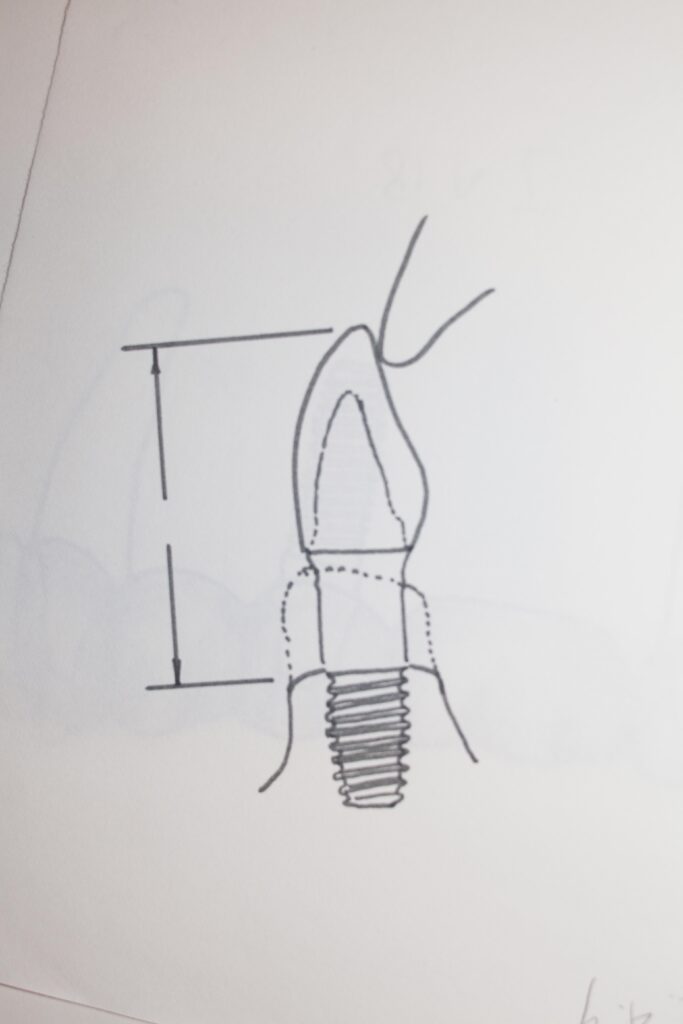
Basically it is a titanium screw, pretty much like you would place in a block of wood. First you drill a hole, then you turn in the screw. In this case, we are VERY careful to make sure that the TIGHTNESS of the screw into the bone is controlled by measuring the torque as it is screwed in – just like using a torque wrench when working on your car – AND we make sure that it goes into the bone the correct distance.
The top of the implant has a threaded hole into which can be inserted a very small, gold, bolt (but in dentistry it is called a screw). This bolt can be used to retain a CAP which covers the implant during the healing stage under the gum tissue, or another type of cap that extends THROUGH the tissue, preparing the form of the tissue to adapt to the crown later. And the screw on top of the implant will later be used to retain an ABUTMENT – which is a metal part to which the crown or bridge will be secured, either by cement or by another screw.
An implant is just an artificial tooth root!
But, the implant must be placed in exactly the right place, with the correct angle, and the boney support of the implant must be adequate to resist the forces that will eventually be imposed on the implant by the prosthesis.
The PROSTHESIS is where the action is. That is where we rebuild the mouth, the bite, the teeth, the appearance, the comfort, and the functionality of the mouth. The implant or implants simply make it possible to anchor that prosthesis firmly in the bone, and will hopefully provide success for the restoration for a long period of time.
There are challenging choices that need to be made before the dentist starts an implant-supported case. The bone needs to be appropriate in every way, the implant choice has to be good and the placement done with skill, and the prosthesis must be designed so as to not compromise the health of the implants in the bone.
If the implants are done well and the prosthesis poorly, the restoration will fail prematurely. If the prosthesis is designed and made well but the implants are placed in bone of poor quality, the restoration will fail prematurely. If the prosthesis is placed on the implants before they are bonded to the bone well, the restoration will fail prematurely.
We’ll see in this chapter how these choices are made in your best interest.
Dental Implants and Prosthetics: The Basics
Planning the Case
When is an implant appropriate? What are the indications and contraindications for an implant? WHO places the implant(s) and WHO designs and delivers the prosthesis?
First – your dentist will be the person with whom you have the first conversation about the possibility of implants. They will tell you that a thorough evaluation needs to be done to see if you are a candidate for this restorative approach.
Second – you will have a detailed scan done of your bone, wherever there will be a need to replace some teeth. If you will be having many implants to replace most or all of your teeth, the entire upper and lower jaws are scanned by a digital system, like a CAT scan, to get all of the needed information. This might be done by an independent laboratory, or by a dentist who does a lot of implants and has the specialized equipment.
Third – based on the information collected, whoever will be doing the implants will make a detailed plan for how the prosthesis will be designed. This MAY be your dentist, but could well be another specialist. This design needs to take into account the quality of the bone, the forces transmitted to whatever prosthesis is needed, and how those forces are transmitted to the bone through the implants.
How Failures Happen
There are times where the dentist will send a patient to someone else to do the implants, and when they are put into the bone, the dentist will have to figure out how to design an appliance that will fit to them. This is an uncoordinated approach, and has resulted many times in failures.
There are oral surgeons and periodontists that place implants for dentists. If things are not planned well ahead of time, they may just put implants where they THINK they will work, but it is up to the restoring dentist to MAKE it work. We will see how this might not be possible.
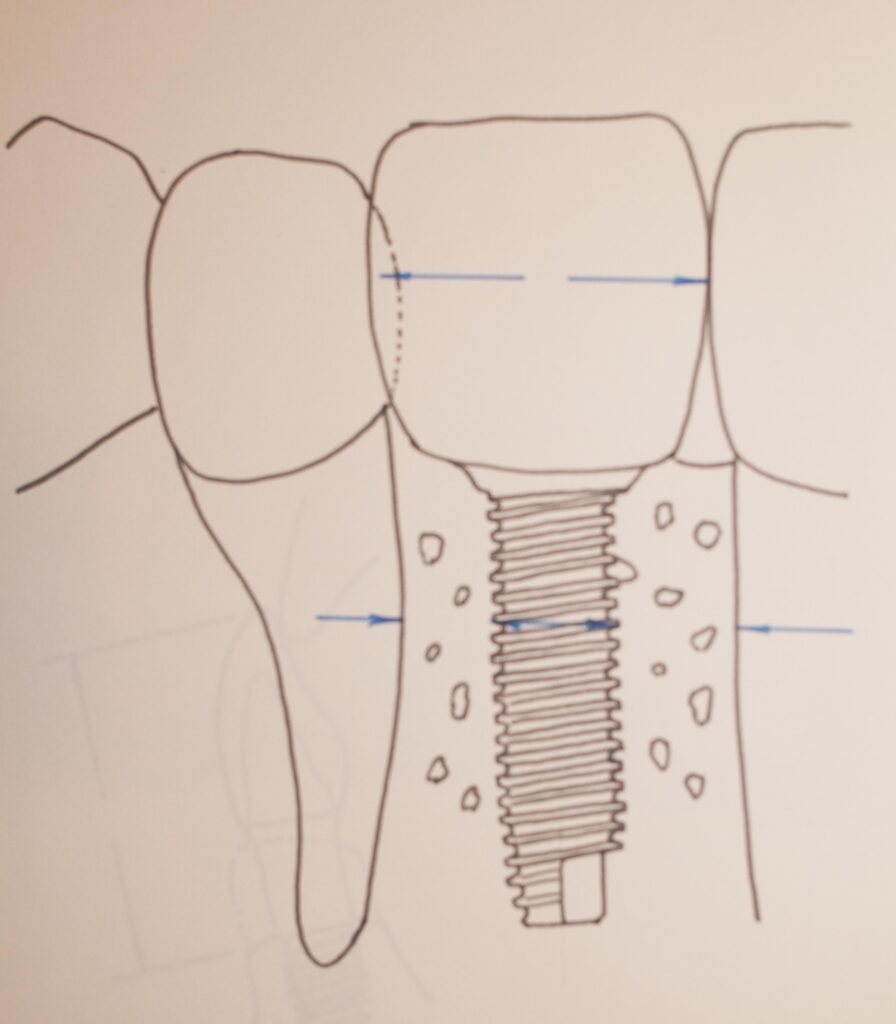
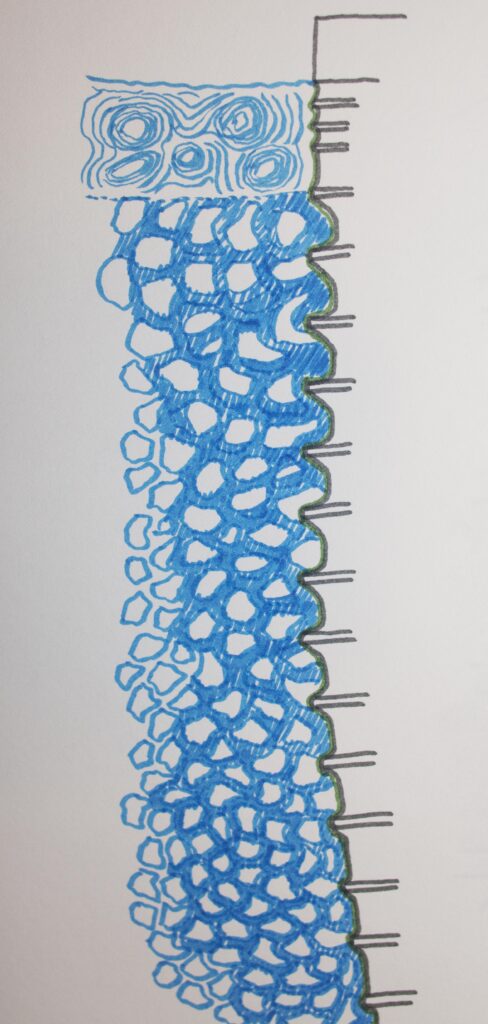
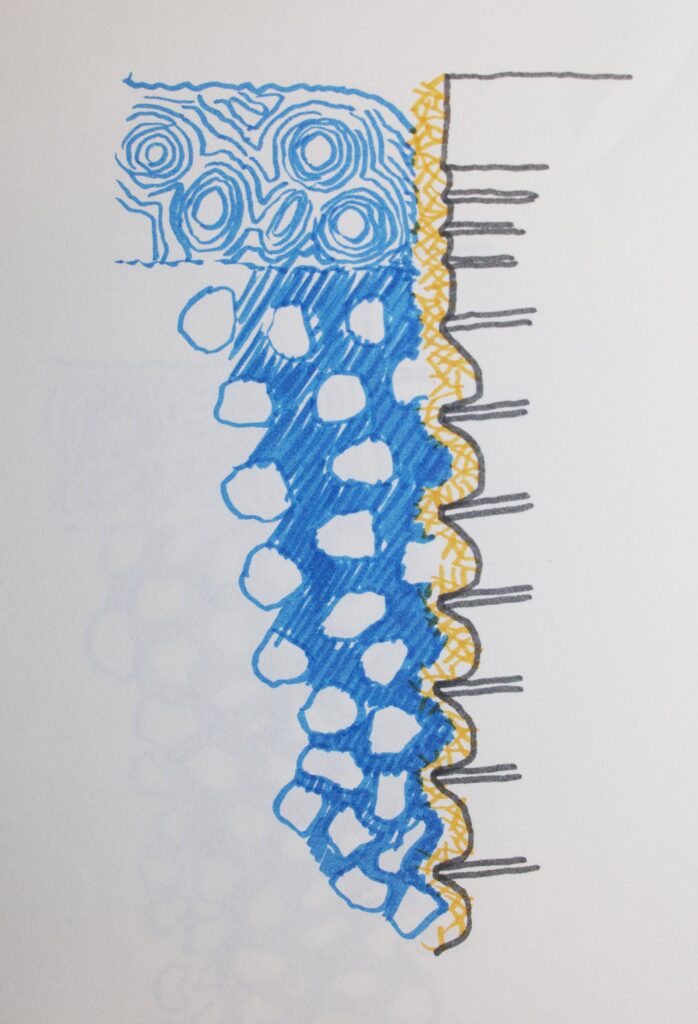
The quality of the bone determines how the forces on the implant are transmitted to the bone. The following two diagrams show that for bone with a dense top layer movement tends to be toward the bottom, otherwise it is toward the top. When the prosthesis is designed, it should take into account the quality of the bone where each implant is placed, so the forces, or loading, is appropriate or within a tolerable range.
Deciding WHO should do the work for you.
It may be that your dentist is eager to do your case. He/she may be well trained and very experienced, or just looking to make a lot of money doing a bridge over a couple of implants, thinking they are like teeth.
Whoever does you work, they should be VERY experienced, and if the work is shared between two or more specialists, they should work TOGETHER in a very coherent fashion so everything is taken into account from the start.
I have a couple of friends that regularly place implants for general dentists. They place the implants in areas that should work well, but when the dentists do the restorations, particularly bridges, they make it so that the forces applied to the implants are too high, or directed poorly. Often there are failures NOT due to the placement, but due to the design of the prosthesis.
Implant-borne prostheses are Expensive!
Every implant will cost somewhere between $1000 to $3000 to place in your mouth, and the abutments are extra, and the prosthesis is an additional $1500 or more per tooth. THAT adds up!
You need to make sure that if your general dentist is doing the restoration, they are well trained and experienced. And you need to make sure that either the same person is doing the implants AND prosthesis (perhaps a prosthodontist specialist), or everyone is totally coordinating their efforts and decisions.
Dental Implants and Prosthetics: The Principles
Indications and Contraindications for Implants
Indications: missing tooth or teeth, history of difficulty wearing removable appliance, many teeth missing in a row, patient will NOT wear partial denture, full denture patient with adequate bone, hyperactive gag reflex, and some healthy teeth in the mouth that would otherwise have to be crowned for a conventional bridge.
Contraindications: Psychological problems, patients with unrealistic expectations, patient having had high dose radiation to head and neck, blood diseases, diabetes, high Blood pressure, bone or soft tissue diseases, inadequate bone volume, excessive use of alcohol, use of recreational drugs, smoker, bone not amenable to augmentation, and the use of certain drugs for osteoporosis.
Even more detailed judgments can be made after a complete workup and assessment of the patient and their specific needs.
Osseointegration
This is the process by which the titanium implant becomes ATTACHED to the bone of the jaw at a molecular level. In the 1960s Branemark is Sweden tried placing titanium screws in animals, and found that sometime later he could NOT get them out! They were integrated into the bone – osseointegration is the term he coined. Think of putting a bolt into some metal and letting it rust for some years – no way you are getting that out. Kind of the same thing.
Many things affect the occurrence of osseointegration. If it does NOT occur, then the implant will fail.
Everything listed here is important: the material of the implant, the surface texture and quality of the implant, heat generated when it is placed, contamination that may be present, the quality of the bone, how well the implant is stabilized at placement, whether fibrous tissue will grow down the sides of the implant, and how much load is placed on the implant.
Each of these things can potentially be controlled, but each determines the success of failure of the implant by affecting osseointegration.
Classification of Cases
Region of the mouth involved
This classification is helpful, because every TYPE of case will possibly, or likely, require a different approach.
- Class 1 – edentulous areas at the back of the mouth on BOTH sides – like the RPD class I case.
- Class 2 – edentulous area in the back of just one side of the mouth – like the RPD class II case
- Class 3 – one side of the mouth with back teeth missing, but an existing tooth behind this edentulous area.
- Class 4 – anterior edentulous area crossing midline – again, like the RPD classification.
Also, depending on where the teeth are missing specifically, there are a variety of things that one needs to watch for. The REGIONS that may require different approaches are:
- Upper Anterior – particularly with respect to ridge position, ability to provide appropriate lip support, possibility of immediate loading of implant because of lower chance of heavy occlusal forces, must watch smile line and appearance of soft tissue relative to implants
- Upper posterior – common problem is size of SINUS and thickness of bone between it and the ridge (not enough bone for implant), typically poor quality bone in this area, distance between upper and lower arches may be SMALL.
- Lower anterior – best quality of bone in the mouth, dense bone may cause overheating during placement, boney ridge may be hollowed out on the facial side, angulation of the ridge and bulk of jaw bone may be different.
- Lower posterior – Arch form can widen as bone has resorbed, and nerve canal in this area requires shorter and wider implants.
Also, fully edentulous arches are classified according to whether all of the boney ridge in which implants will be placed is at the same height or not. These differences may have to be compensated for by bone grafting certain areas to make the uniformity of implant support better.
Bone Classification
The nature of the bone will determine how feasible a case may be. We will look specifically for all of the following characteristics:
- Bulk or quantity of bone – there needs to be enough bone to support an implant of adequate length and size
- Density or quality of bone – if the density is low as it often is in the back of the upper arch, it may not provide much support to the implant, and hence to the prosthesis.
- Homogeneity of the bone – is the bone more dense in some areas and less so in others? This could complicate siting of implants.
- Angulation of the ridge of bone that supported the teeth and now must support the implant. If the implant would need to be placed parallel to the ridge, but the ridge is not pointing toward where the abutment should be for the arch form, that is a limitation.
- Position of the ridge relative to the desired form and position of the teeth in the arch. If the ridge is not where the teeth should be, the implants would have to be placed at an angle, which may exert forces on the implants which compromise osseointegration.
- Changes in the boney ridge recorded over time – if the ridges have been shrinking over time (under dentures, for example), is the thickest part moving inward?
Existing Structures
- Are there failing teeth that should be removed before implants are placed?
- Have the edentulous areas been without teeth for a long period of time? That determines the level of bone in the area.
- Is the occlusion or bite in the patient likely to exert strong forces on the replacement teeth?
- Are there nerves or sinuses in the bone that need to be avoided as the implants are placed?
Design Concepts for Prosthesis
Many things need to be taken into account when designing a plan for a prosthesis involving implants. We will list these below.
Complications with bad Design
When the design and planning for the case are poor, complications may well arise. these complications can be:
- Implant fails to osseointegrate and is not held firmly in the bone
- There is bone loss around the implant so the support is diminished
- There are fractures of materials in the prosthesis, particularly those involved in occlusion
- Some of the components of the implants may fracture
- The restoration will not be retained
Things which influence the design of the Prosthesis:
- Existing occlusion – materials to restore occlusal surfaces, relationship to hinging of the TMJ, need to extract teeth that will interfere with plan.
- Interarch Space – between the upper and lower teeth. There must be a minimum of 7 mm for fixed restorations and 8 – 10 for the anterior teeth. Removable appliances require more. Long-term denture wearers typically have very little space available unless the bite can be opened up, which means restoring everything.
- TMJ – needs to be comfortable in movement, with no deviation side-to-side or limited opening.
- Existing prostheses may be in place and will continue to be used – they must be evaluated for any changes that should be made in function or esthetics.
- Arch form – some people have a fairly square arch, and some are more pointed or tapered – but typically ovoid in shape. This shape will determine much about where implants should be placed and how the prosthesis should be made to reduce maximum forces on imlants.
- Tooth location and condition – if the second molar is missing, it will rarely be replaced by implants because most of the chewing function occurs on the first molars. And second molars can often lead to interferences in forward and backward jaw movements.
- Lip line at rest and during speech – the esthetics are determined by what CAN be seen as the lips are positioned in various expressions. Often the design of an implant-borne prosthesis must take this into account.
- Mandibular flexure – for people who have little alveolar ridge left on the jaw – and bone resorption besides – the jaw can be very THIN. If it is thin, then it can bend under various forces. If it can bend, then FIXED prostheses that are connected to it will be stressed where they are connected – the implants.
- Soft tissue support – especially for implant retained dentures. While the implant remains fixed in the bone, the denture which is connected to it may move as it sits on soft tissue, especially when the tissue recedes over time. Frequent reevaluations need to be made.
- Need to support prosthesis on implants AND natural teeth – this can be considered if the expected lifetime of the tooth is more than ten years – it should have little restoration already and be well supported in the bone, and NOT mobile. When the tooth can be made to move visibly, and the mobility of the tooth and implant are different, problems ensue.
- IF the prosthesis is built on THREE supports (abutments), if the end two are natural teeth and the middle one is an implant, that is not a recommended approach. The prosthesis will end up rocking on the implant, exerting harmful forces.
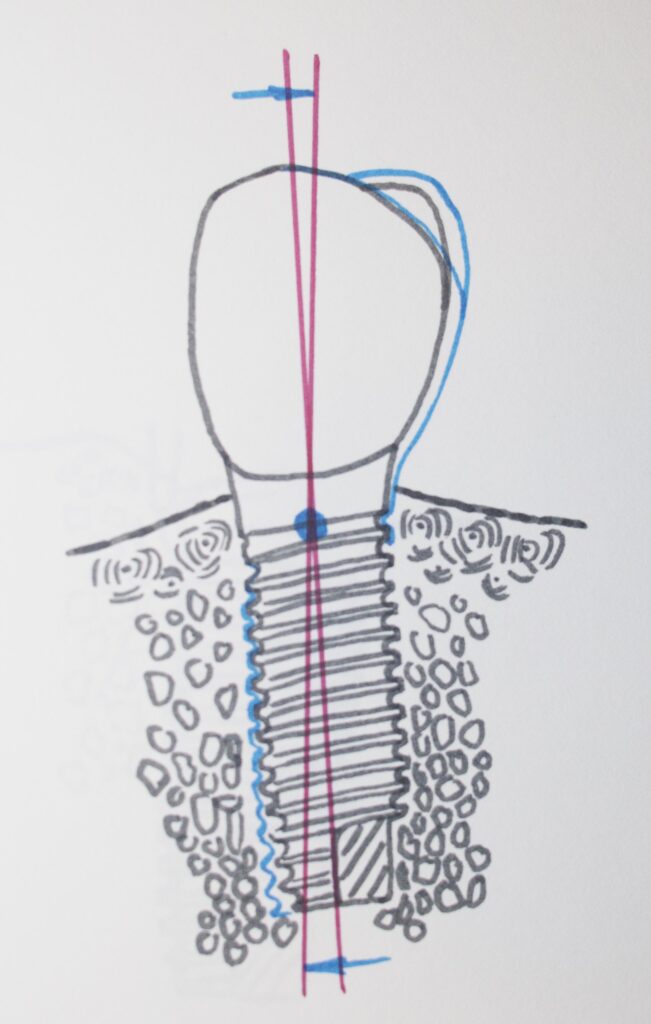
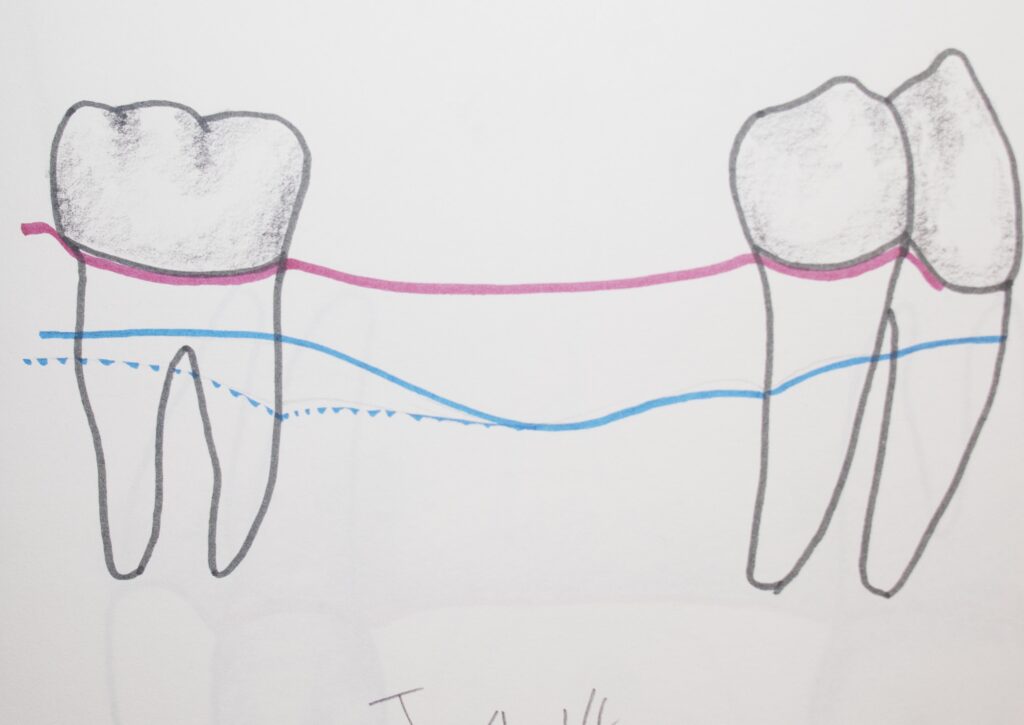
- Crown-root/implant ratio – the length of the implant embedded in the bone must be at least twice that of the crown above the bone. Otherwise there will be a harmful leverage of forces applied to the bone. This is also true when the prosthesis is supported on a tooth.
- Endo on natural teeth? It has been suggested that any tooth that is used to support a bridge WITH an implant be endondontically treated first. If there is a need for a RCT after the bridge is cemented, it may compromise the entire prosthesis to do it.
- When only implants support a bridge, it can be secured to the abutment teeth either by cementation or by screwing into place and sealing the holes. If the prosthesis needs to be replaced it can if it is screwed in. But, these prostheses need to be thicker than ones designed for cementation, and there may not be enough room for them.
Loading of Implants
Success or Failure?
The success of an implant-borne prosthesis depends largely on how it responds clinically, mechanically and microscopically to forces applied to it in the mouth.
Success of implant: it is a stable and immobile support under load and there is no pain, inflammation or loosening. There is no relative motion under load for the life of the patient. The mineralized bone tissue makes intimate contact with the implant at the interface – i.e. it is osseointegrated.
Success of the prosthesis: The prosthesis exerts the appropriate load, under function on all implants. AND – this load is in the appropriate DIRECTION on all implants.
Failure at implant: Excessive relative motion develops, screws loosen or break, and there is observed fibrous tissue at the implant site.
Failure of prosthesis: Functional overload from prosthesis leads to loss of osseointegration. Or the stress at the implant is too LOW, causing the bone to resorb due to dissuse. The porcelain of the prosthesis fractures or the framework fractures. There is loosening of any natural teeth involved.
Determinants of Load
- Occlusal forces – the bite. The pressure we are capable of exerting with our bite is a LOT. And, the LATERAL force can be about 10% of the vertical force, if we have grinding habits. That is potentially very damaging. The more tooth surface this load is spread over, the less will be the pressure that can be concentrated on one point.
- Effect on Prosthesis: It can bend, it can twist, and these forces can even have a component in an UPWARD direction if there is a pivot point or fulcrum in the prosthesis.
- For single tooth replacement, the off-axis forces are minimal and the resistance to occlusal loads with strong bone is optimal. Longer implant-supported bridges require more rigidity and careful design. Sometimes part of the prosthesis must be left hanging out beyond the last implant, as a CANTILEVER. Without careful design, damaging loads can be exerted on the last implant.
- Forces OFF the AXIS of the implant, will tend to cause it to tilt – and this can damage some implant components.
- The forces and torques exerted onto the implants by the prosthesis are countered by the bone – and these must be balanced forces. If there is a loss of bone, the balance will be thrown off and failure can result.
Mechanical Models
It is possible to construct mathematical models to estimate the forces that are exerted on each implant by particular designs. However, the reality of the situation in the patient’s mouth adds many variables and the problem is not likely soluble in detail. Generally, it is the experience of the dentist who can use his/her best judgment to determine what is needed to do a successful job.
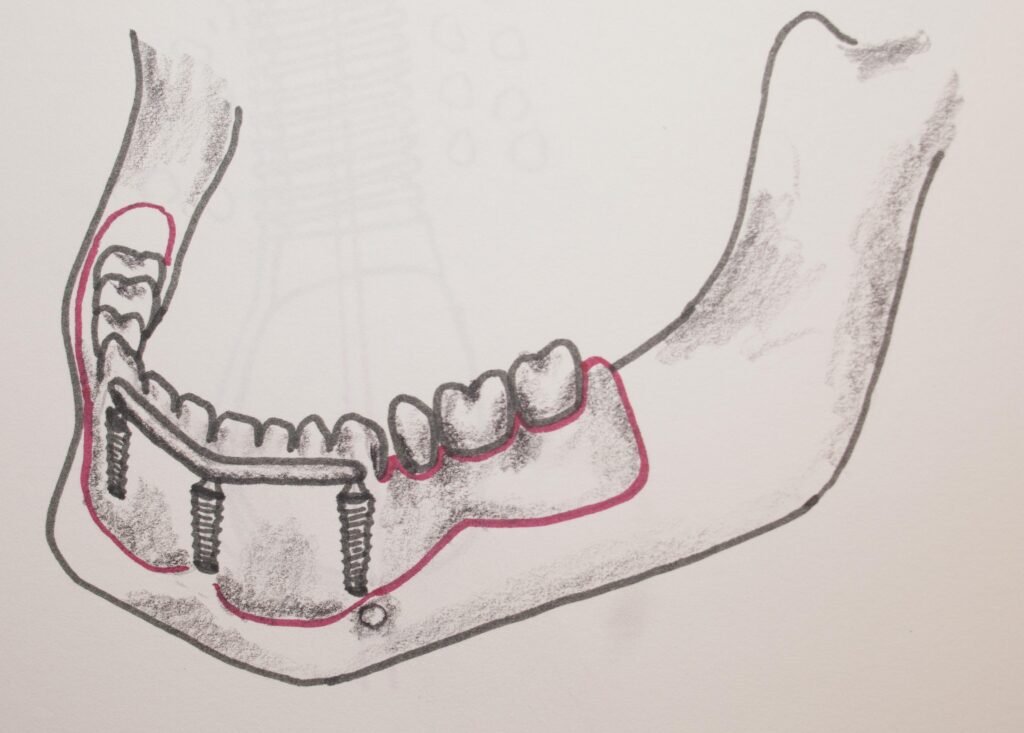
One of the decisions that might have to be made is how to support a complete arch prosthesis, say for the upper arch – deciding between using four or six implants.
With four implants there would be a cantilever on each side, and the possibility of tipping forces across the arch, whereas there will be less of a cantilever for 6 implants, possibly, as long as the bone further back in the arch is suitable. If the implants in either case have to be restricted to the same area of bone – just more implants in one case – the pressures and tension forces are not that different. That is why the building of full arch prostheses on four implants – “All on Four” is often successful.
Calculations for the use of ANGLED IMPLANTS have also been done. Implants can be placed in the bone at an angle to reach further back in the arch, so the cantilever will be less. But – the forces on the implant will tend to be OFF AXIS, and if they are strong enough can compromise osseointegration. On the other hand, for an angled implant there are occasions where the implant can engage BOTH the strong outer bone where the implant enters the bone, AND where the tip ends up. THIS is a very stable situation. The mathematical models of this are probably not accurate enough to make good judgments, but suggestive that it is “worth a try”. The try has been done and is often successful – but a long implant must be used and placed very precisely.
Other factors that make reality different from calculations:
- The implants are flexible to some extent.
- The implant may be somewhat mobile in the bone.
- The framework of the prosthesis can FLEX. In fact, acrylic frameworks between implants flex more, and the loads transmitted to the implants are somewhat less as a consequence.
- The relationship between the forces exerted on the prosthesis ON the implant, and the forces WITHIN the implant that hold the abutment to the implant must be considered. If the outside forces are larger than the torque applied to the screws within, things can loosen and move.
- The INTERNAL load of the implant that can be achieved is determined very much by the FIT of the prosthesis to the implant/abutment. As things are tightened down, if there is a gap or angle between two mating surfaces, a significant torque cannot be achieved and the low internal load will cause the assembly to loosen.
Bottom line:
The design of the implant system and prosthesis must be carefully considered so that allowable limits are not exceeded.
Allowable limits can vary from patient to patient, depending on exact bone condition and bone response to stress and the patients movement and functional habits.
A lack of precision in fit can easily compromise the success of a case!
Placement of Implants
A general dentist can go to a manufacturer’s course for a weekend and learn how to place an implant! They get a Powerpoint presentation and take some plastic bone models and install the implants that the manufacturer is selling. The early “Weekend Warrior” course has mislead many dentists over the years. It seemed that if you can get the implant in the right place at the right angle, you can probably install the correct abutment and make a crown. Done deal.
But – even for single tooth replacement implants, the choices and skills for implant placement and restoration are more subtle than can be taught that fast. Many general dentists take what is called a “Maxi Course” – which is an extended program ranging from lectures and study course material, through plastic bone models to animal bone models to patient experiences.
But, while implantology is not a recognized specialty, as is prosthodontics, endodontics, oral surgery, and periodontics – it is pretty close. All of the above specialists MAY choose do to implants to bolster their practice income, but the prosthodontist, who is a specialist in the design and installation of prostheses, on natural teeth or on implants, is the only specialist that will likely do the whole job.
But, again, there are general dentists out there as well who have made it a point to get well educated in the field – and there are advanced education programs specifically in implantology that are very thorough.
The issue at hand is that for any implant case the cost is VERY high – and it behooves one to search out the best practitioner there is to help you decide what to do, and to do the work for you.
Single Tooth Replacement
This is generally a pretty simple situation, a tooth is missing, place an implant and a crown and voila! But not always. The bone level in the edentulous area is critical, and the structure that may lie beneath the implant, a sinus or a nerve, are critical as well as how much bone there is to support the implant. And, of course, the density of the bone.
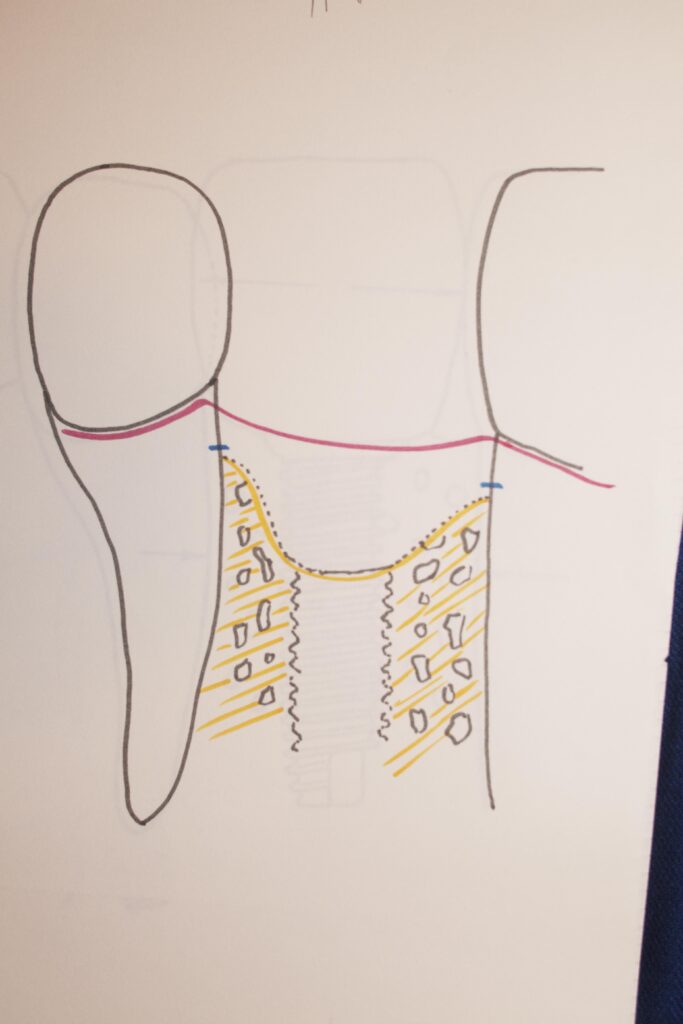
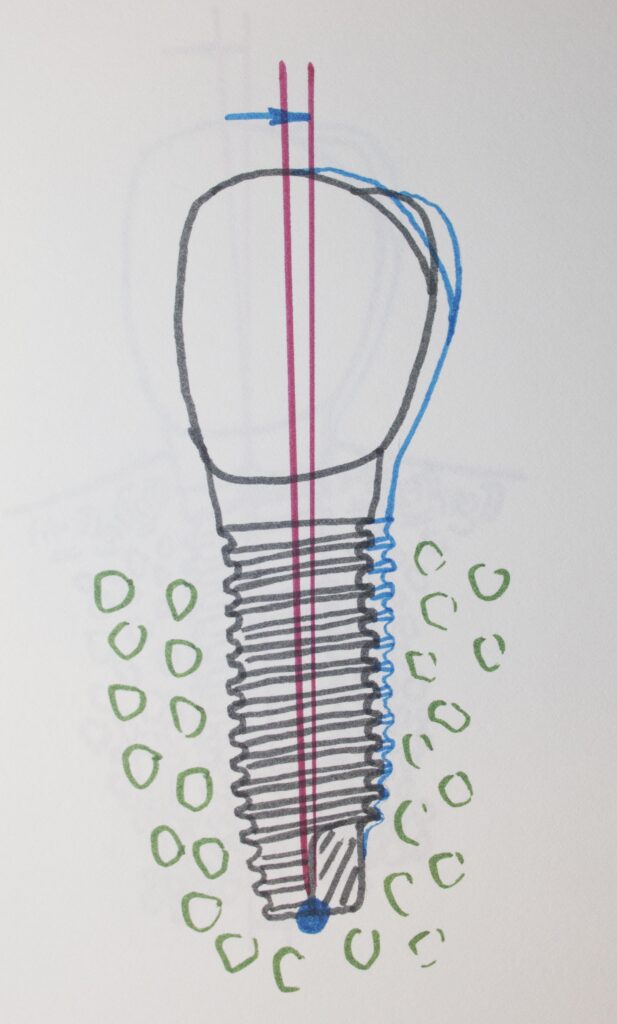
If the tooth has just been extracted and the socket where the tooth came out is not too wide and an implant can be found that is wider, but not too wide for the space between the teeth, then the implant can be placed, along with some bone graft material as may be needed to fill in around the implant, and the whole thing sutured over for a few months to osseointegrate.
There are three different types of implant placement techniques. First is simply drilling a hole and then screwing in the implant. When the bone is not too dense, this typically works fine. Second: If the bone is more dense, it will be necessary to TAP the hole – use a tool to create threads inside the bone that the implant can screw into. This is then like screwing a bolt into a threaded hole in a piece of metal. The third technique uses an implant that has no threads, but is bare on the sides, and it is PRESS-FIT into a very precise hole that is drilled for it in the bone. Any of these techniques can be used in various situations, and it is up to the dentist to decide what is likely to give the best result.
It is important with the threaded implants that the torque with which they are seated is to a certain level, not too little, and not too much. Upon this rests a lot of the success of the osseointegration. The dentist actually uses a little torque wrench to place the implant.
In general, when the implant is osseointegrated and uncovered and an abutment screwed on, some preparation of that abutment may be necessary for the particular type of crown desired, and then an impression is taken for a crown made in the usual way – which is eventually cemented on. It is also a choice to have a crown made to a metal coping that is an exact fit to the abutment, which has a threaded hole so the crown can be screwed down. The esthetics of the situations may be significantly different in certain cases, but IF the crown at some point needs to be removed and repaired or replaced, it is much easier with the screwed in crown.
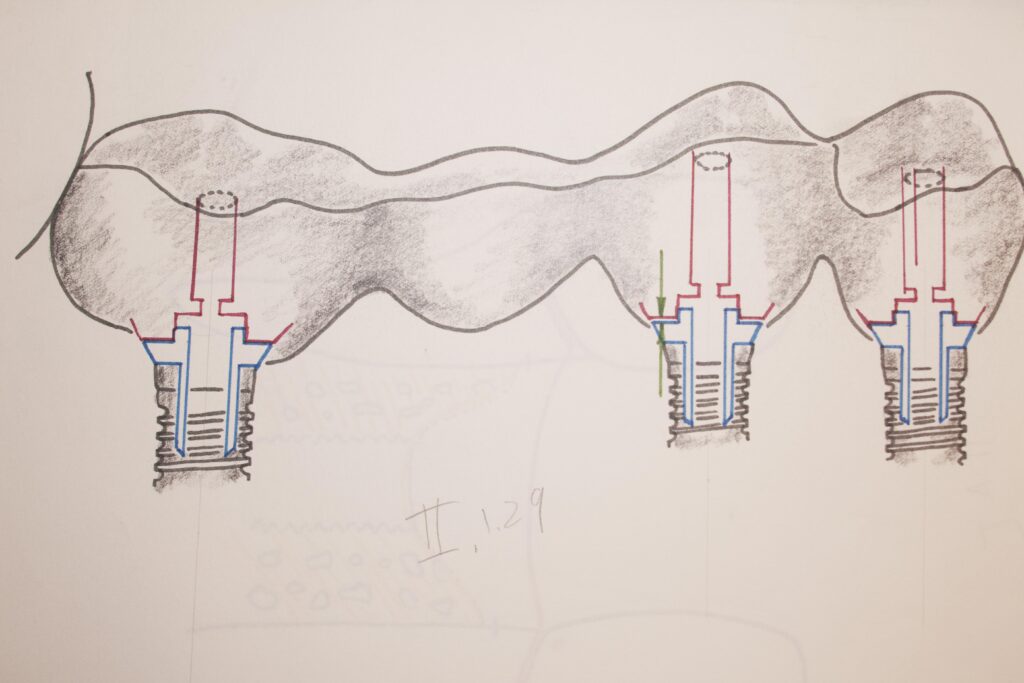
Multiple Unit Implant-supported Bridges
In this case the situation is a bit more tricky. If there are two implants and two abutments and a rigid framework between them, as we have seen, the FIT of the framework to the implants is critical in determining the security of the framework ON the implants, and the forces applied to the implants. Once the two, or more, implants are placed, the impression must register EXACTLY the location and direction of those implants. This is done by screwing a special tube onto each implant, and these tubes are picked up by the impression and transferred into the plaster models that are used to make the framework. This is very exacting work – and the PLACEMENT of the implants must be such that the abutments will be directed in just the right direction so a framework CAN be made!
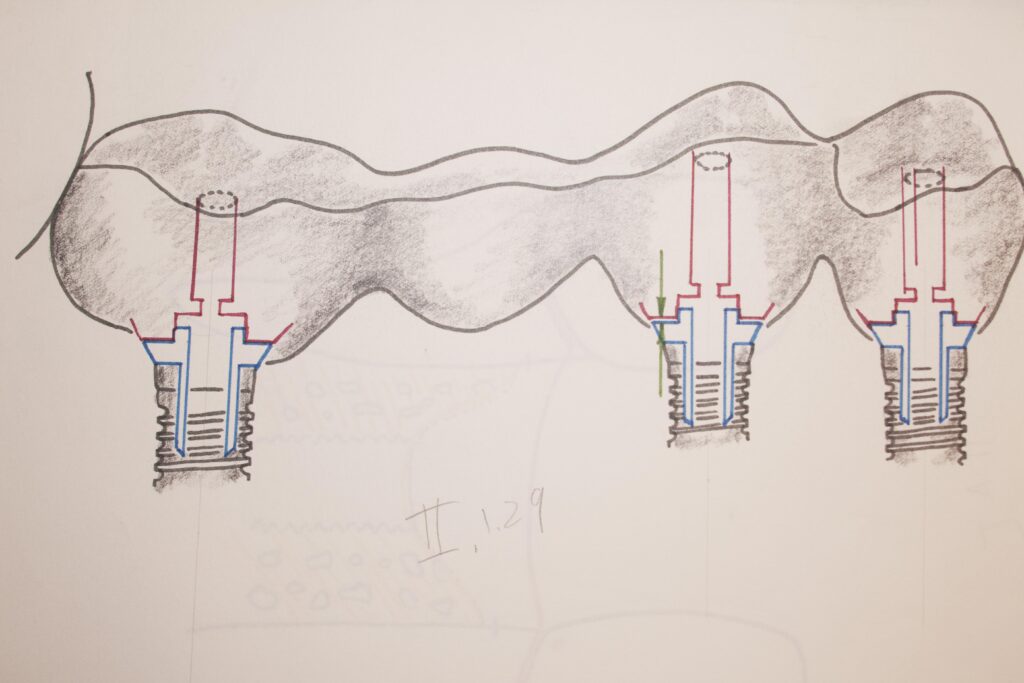
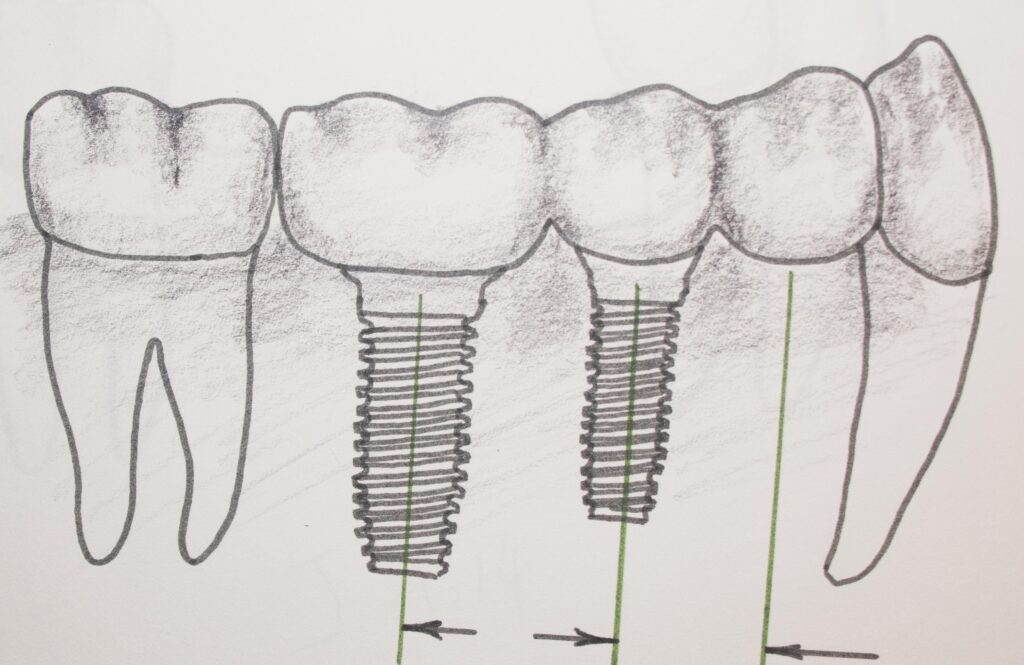
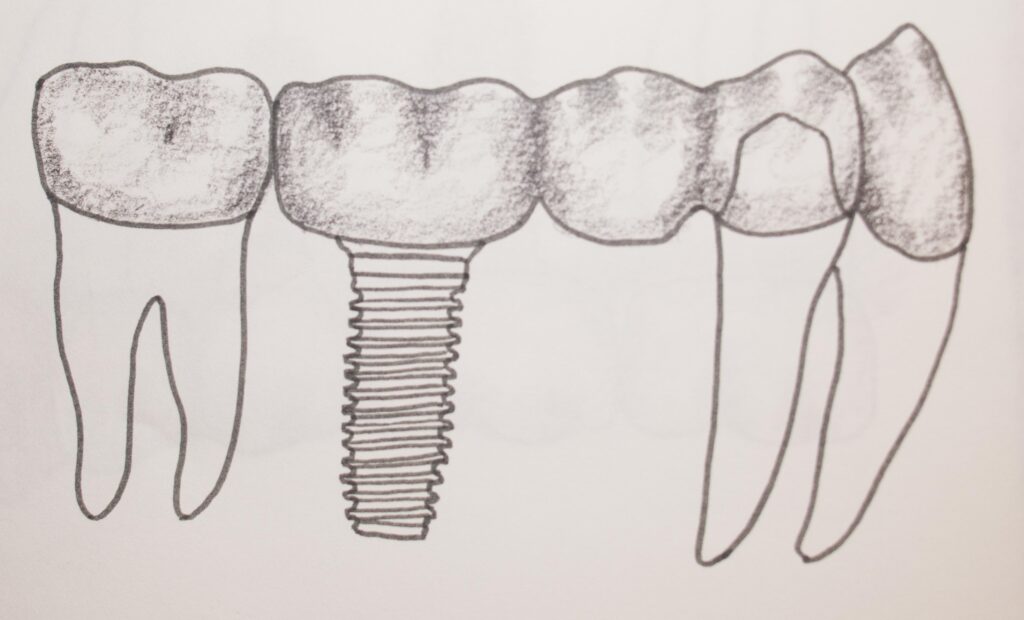
Each of the situations shown above has its challenges. But all can work successfully if the case is designed well, the implants are placed well and great care is taken to make sure the metal framework of the bridge fits on each abutment with precision. Any lack of precision can compromise the success of the whole case.
Guided Placement of Implants
This is a very precise way to place multiple implants and have their relationships assured from the start. It is a technique that can be used well by less experienced practitioners. The Guide or Stent that is used is expensive to have made, and subtracts from the profit of the procedure for the dentist, but in tricky cases it takes a lot of the “guess-work” out of the placement.
The surgical guide can be made in a variety of different ways these days. Optical scanning of the tissue, CAT scan imaging of the bone, 3D digital printing – all work together to produce the guide in the lab. The guide can even be made so accurately that a bridge can ALREADY be made, ready to place once the implants are installed!
How does THAT work? The guide has metal sleeves embedded into it for the implants to be screwed through into the bone, in a particular position, at a particular angle, and to a particular depth – exactly!
The dentist places, very securely, the guide in your mouth (it may even be tacked to your boney ridge for perfect stabilization) and drills through the sleeves into your bone, to an exact depth. Then he/she puts the implant on a torque wrench and turns it into the hole slowly, and the plan is that it will get to a good range of torque JUST as it seats completely in the guide to the upper surface of the sleeve. This insures that the implant is at the correct depth, as well as torque, as well as position and angle.
If the dentist has placed two implants in this way accurately with the guide, so that the placement of one implant has not altered the position of the guide in any way, the relationship between the first and the second can be so accurate that a pre-made bridge can be screwed or cemented to them immediately.
Teeth in an Hour
This is where the dentist has opted to use a surgical guide and placed the implants according to it, while the lab that made the guide made a matching restoration as well. This takes a lot of data for the lab to get things right, and the dentist has to use the guide perfectly. Imagine the precision of fit that needs to be met so that each of the crowns that support the bridge exactly mate with the abutment which is screwed to the implant! The slightest deviation, far less than a degree of angle, can result in unsupportable forces being applied to the implant, and eventual failure. And, the contact with any adjacent teeth needs to be good, as well as the contact with the opposing teeth. Of course the dentist can adjust adjacent contacts and opposing ones a bit, but the lab needs to get it pretty close.
But, when all goes well, the patient comes in with no teeth and leaves with teeth – in as little as an hour!
Is this always the way to go? For really big, complicated cases, it may be unwise even for an experienced practitioner. But it certainly has some advantages for the patient. The placement of the restoration on newly installed implants is not always appropriate, depending on the bone levels and density, but many times the situation is amenable to this approach.
Home Care of Prostheses on Implants
One of the reasons dentists need to evaluate a patient’s home care before embarking on an implant restoration is because implants really do require great home care!
Remember, this is a piece of metal that is anchored in your bone and extending into a place filled with potentially harmful bacteria.
Besides brushing and flossing any areas that you can, cleaning the space underneath the framework or crown where the gingiva makes a seal around the implant, is crucial.
You may use electric toothbrushes, water jet type irrigation devices, and little bottle-brush like brushes to good effect.
Your dentist may well prescribe a strong mouth rinse as well, especially one made with chlorhexidine, which is very effective in eliminating bacteria that cause gum disease, and can protect the seal around the implant very well.
And – of course, pay attention to how your implant-borne prosthesis is acting. Is it rocking, does it hurt to chew on it? These are things that need to be called to the attention of the dentist immediately. Also, make sure that every recommended follow-up appointment is kept – these are not teeth and will not take kindly to the types of abuse to which many people subject their teeth!
Bottom Line for Dental Implants and Prosthetics
Implants have been a real boon to dentistry over the last few decades. Many things have been made possible that would otherwise not have found a good solution.
Implants are not for everyone.
Implants are not for every case.
Implants are not for every dentist – and some cases require the work of only the most experienced and devoted practitioner.