If you would like to explore more on the subject of TMJ disorders you might check the webMD website on this subject. For a more detailed treatment of orofacial pain you might explore with Wikipedia article on the subject – there are ample references to the primary literature if you want to dig in deeper.
Organization of this Chapter
You May Skip to Whatever Subject Interests You Now
Basics
TMJ Disorders
Functional Disorders
Inflammatory Disorders
Other Orofacial Pains
Muscular Pains
Vascular Pains
Sinus and Nasal Pains
Nerve-Related Pains
Bottom Line for TMJ Disorders and Orofacial Pain
………………………………………………………………………………………………………………………..
TMJ Disorders and Orofacial Pain: Basics
In this chapter we are definitely biting off more than we can chew, even if chewing does not cause us any pain! Just the subject of TMJ disorder has become so popular that whole books have been devoted to the subject, and there is much disagreement about the causes and treatment, even amoung experts and authorities. Orofacial pain includes all other pains in the region of the face, omitting coverage in this chapter of dental and periodontal pains which are discussed elsewhere.
While TMJ disorders are really a subclassification of orofacial pains, they are given sepatate billing due to their public notoriety and to the fact that, as a joint, the TMJ is susceptible to a variety of problems that the other tissues are not.
We will first discuss the TMJ and its problems – the treatment options will only be mentioned, as they are beyond the scope of this site. The other kinds of orofacial pains will each be mentioned here including some idea as to the appropriate therapies.
It must be borne in mind that I am not by any means a well-informed source on these subjects. They are complex issues and require individual attention and evaluation, and mostly these issues are beyond the training of a general dentist. I know enough to find a person that can help a patient in need, and I can introduce these subjects to you now in cursory detail.
TMJ Disorders
It must be noted that when one says in popular parlance, “I have TMJ”, it means nothing. It’s like saying “I have a knee”, but it is meant to convey to the listener that there is a PROBLEM with the TMJ. More correctly, one could say “I have TMD” – temporomandibular dysfunction – or just spell it out.
We will divide this section into two parts: functional disorders and pain syndromes. The functional disorders are related to irregularities of joint movement, and these irregularities can result from congenital deviations in anatomy in the region of the joint, or from alterations that occurred as a consequence of abuse or trauma. The functional disorders may or may not be associated with pain. There are several painful problems, however, that are not disorders of function or movement, but are specific to the joint tissues. An example would be arthritis of the TMJ.
Functional Disorders
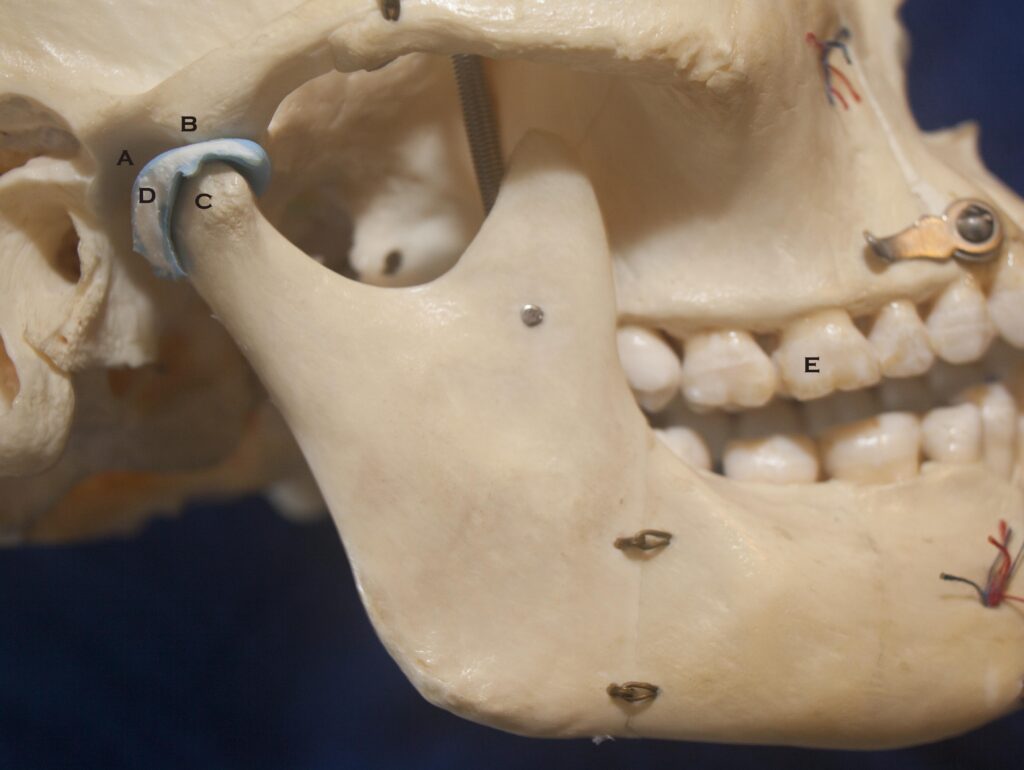
The symptoms of these disorders are normally related to a defect in the structure or characteristics of some component of the TMJ complex. In general there may be a non-ideal relationship between the condyle and the disc. (See the picture below for the labeling of components of the joint complex). The cause of this abnormal relationship or derangement is often unknown, and the situation is often evolving with time, but some particular examples can be given.
If you have clicking, clunking, or grinding noises as you open and close your mouth, you probably have a TMJ derangement. Depending on the precise condition you may never be bothered by it, may at some point develop pain associated with moving the joint, or be in frequent extreme pain.
One hypothesis is that hyperactivity of the muscle which connects the TMJ disc to the bone behind the upper wisdom teeth can cause the disc fibers to elongate, thinning it out and allowing increased sliding movements of the condyle over the disc. It is possible that a tendency to have a flatter condyle working against an angular fosse can also contribute. Eventually the condyle can assume either of two positions on the disc, one toward the front and one toward the back. In this case, the ability of the disc to slip back and forth during jaw movement will cause a sudden click in each direction. This RECIPROCAL CLICK is fairly common, and when not heard can often be felt with the fingertips during opening and closing motions. If the situation progresses to the point where the condyle can rest behind the disc on the supporting fibers, pain can result due to the presence of nerves in these fibers.
If the problem evolves further then occasionally the disc can perforate so that the condyle is functioning against bone, or it may ride constantly on the fibers behind the disc. Either of these situations is difficult to tolerate.
Other kinds of clicks are often encountered. There are single click situations, and also double clicks that occur at different positions of the jaw, each of which can be associated with a type of disorder by the experienced clinician.
The opening “thud”, or “clunk” is also fairly common. It is associated with a sudden jump in the condyle position as the mouth is opened. It is mostly associated with an unusually steep fossa slope that the condyle rides on during the initial phase of opening, followed by a sudden transition to a flat section. It is generally not related to a specific disease process.
Ever know someone who opened their mouth, perhaps to yawn, and couldn’t close it again? This is referred to as spontaneous dislocation. It is a joint dislocation, just as sometimes happens to shoulders and knees. It can occur in anyone, but is most common in the “thunkers” mentioned above. It is caused by movement of the condyles so far forward out of the fossa that they get stuck. Generally, strong downward pressure serves to return the condyles to their proper place – usually by a second party. I’ve had to do this with a patient in the dental chair.
So what causes these disorders of function? It could be anatomical, where the relative shapes of the condyle and fossa are important. Or it may depend upon how tight the ligaments are that keep the joint together. Or perhaps it has to do with hyperactivity of the muscle that attaches to the disc, or to what extent this muscle pulls on the disc rather than the bone. And, on top of all this, stress probably plays an important role, for discomfort from any of these abnormalities can be exacerbated by stressful situations. And, if we needed something else to concern us, the way the teeth come together is important, because they might not come into occlusion when the joint is in its most comfortable position. Visit Chapter II.5 to learn more about the bite. Also, it is important to note that not everyone is the same with regards to their sensitivity to painful situations. That small disorder that is a minor irritant to one person can drive another person absolutely nuts!
What you ought to take away from all of this discussion is that TMJ disorders can have lots of causes, contributing factors, and symptoms. Worse yet, a lot can be known about the condition of a patient’s TMJ and it is still hard to predict whether it should be bothering them now or whether it will in the future. You might already suspect that any thorough treatment plan will involve a lot of thinking and a lot of disciplines!
Inflammatory Disorders
Disorders that fall into this category are not simply structural abnormalities as we discussed above. Structural abnormalities may cause trauma to the tissues, and the inflammatory reaction to the pain in these traumatized tissues can actually cause MORE structural changes. A true vicious circle!
The pain felt as a result of inflammatory disorders is generally felt as a constant dull ache which is accentuated by joint movement, but it is not the movement that originates the pain.
Inflammation is the body’s response to some kind of tissue disorder, either disruption of cells due to trauma, or disruption due to the presence of an infectious agent. Or inflammation may start in a joint when it is not appropriate, due to a disorder of the immune system, causing it to over-respond.
The four types of disease that are recognized in this category are related to the site or nature of the problem. Inflammation of the joint capsule or lining is generally caused by trauma, for example getting hit in the chin when your mouth is slightly open. Inflammation of the fibers behind the disc can be similarly due to major trauma, or can be caused by intrinsic trauma. Intrinsic trauma is due to a more forward placement of the disc so that the condyle functions frequently on supporting fibers. This chronic, continuing, daily trauma to the fibers often causes inflammation.
The third type of joint disease is called degenerative joint disease. It is not strictly an inflammatory process, but leads to a gradual breakdown of the bony structure of the joint. It is thought to be caused by overloading of the joint, which could be associated with a displaced disc or by increased muscle activity, or both, Again, the increased muscle activity could be due to stress.
The fourth area is true inflammatory arthritis, but this could be associated with either trauma, infection, immune problems (rheumatoid arthritis), or gout. These diseases can cause so much damage to the TMJs that it may have to be replaced with artificial joints.
Other Orofacial Pains
There are at least six other categories of orofacial pains, clearly more than we can look into here in any detail. We will discuss some of them briefly. It should already be clear that when you experience a particular kind of pain in the face it can be a very involved process to sort out the cause!
……….Muscle Pains
Other than dental pain, muscle pain is the most frequent cause of pain in the head and neck region. Even when the primary pain is due to something else, the muscles often become involved as pain in the area sets off excessive stimulation of the muscles.
Muscle pain can be due to excessive stretching, forceful or sustained contraction, lack of oxygen getting to the muscle tissue or trauma and inflammation. Or the pain could arise from the blood vessels in the muscle or from membranes which bound the muscle tissue. It can range from a vague tightness to excruciating agony. To add to the possible confusion, even when the pain in the muscle itself is relatively mild, the way the nerves are connected can make it SEEM that something else hurts when there is nothing wrong with it. It is even possible that pain can be REFERRED to the muscle from some other side, making muscle pain the major complaint, when it shouldn’t be!
We are familiar with the common tension headache, typically affecting the temporalis muscle over the temples. Many other muscles in the head and neck region can give similar symptoms. Treatments can consist of restricted activity, deep massage, local anesthesia and stretch manipulation, ultrasound, use of muscle relaxants, biofeedback, use of anti-inflammatory drugs, deep heating, or increasing awareness of movement during the day using the Feldenkrais modality, depending upon the particular case.
………. Vascular Pains
This category includes the common migraine headaches, but also applies to pain involving other blood vessels in the face and neck region. These pains generally have a pulsing or throbbing quality. There is a lot of variability in this classification of pains, and many subclassifications. Mostly, it is thought that these pains have a strong emotional or stress-related influence. And, even though these are classified as vascular in nature, they can be influenced by awareness of muscular activity in the area.
Treatments include pain relief, fairly heavy-duty drug therapies, relaxation techniques, dietary supplement therapy with L-tryptophan, psychotherapy, and even neurosurgery depending upon the particular case. Again, it is obvious that competant or even inspired medical consultation is crucial in these cases.
………. Sinus and Nasal Pains
People often come to the dentist when they have a pain in the general area of the upper molars. It is possible, however, that the origin of the pain could be in the maxillary sinus into which the roots of the upper molars often intrude. The sinus itself, however, is generally not the primary source of pain, for the lining of the sinus is nearly insensible to pain. Any dental infection can spread to the sinus, and sinus infections can spread to the teeth, however. Also, sinus infections can spread to the nasal membrane if the opening between the areas is not closed off, and there can be substantial pain emanating from the nasal tissues. There can also be referred pain between these different regions, making you feel you have one problem when the cause is otherwise.
Diagnosis is often made by anesthetizing the teeth or the nasal membranes and evaluating the condition of the pain in various areas. One must be careful not to perform unnecessary dental procedures like root canals and extractions until the source of the pain and its cause have been localized to the teeth. Likewise, one must be certain that the teeth are checked very carefully in any case of “sinus infection” or “sinus headache” that is reported.
………. Nerve-related Pains
These pains are not a warning sign of any infection or disorder in any of the structural or supporting tissues. They are caused by a disorder in the nerves themselves. Unfortunately, the pains of nerve origin are generally the most excruciating pains that we can ever experience, and often the cause and cure are completely unknown.
The most well known and most painful of these conditions is called Tic Douloureaux, or trigeminal neuralgia. It generally expresses itself as a lancinating pain in the facial region, following the branches of a particular nerve, stimulated often by a light touch to the sensory area of that nerve. Treatment often involves major surgery to remove portions of the nerve, sometimes deep inside the head!
Neuritis, or nerve inflammation, is another important category. Any infection in the head and neck region, whether extending from the sinuses or from a site of extraction, can spread to nerves. The pain felt in these affected areas is often described as persistent, unremitting, and burning. While the pain can be in the region of a tooth, for example by spread from a sinus, the quality of the pain is different from that of a toothache caused by pulpal infection. It is important to make this distinction, again to avoid unnecessary extractions or root canal treatments.
TMJ Disorders and Orofacial Pain: The Bottom Line
It should be clear that when a patient has problems with the joint or pain in the orofacial region, the diagnosis of the CAUSE may be very complex. As I said, it can take a particularly inspired dentist or physician to navigate the possibilities and know what is best to do, if anything CAN be done.
Let’s hope that you do not have any issues with these extra-oral tissues!
The wise dentist will have physicians that are experienced in this region, and dentists who specialize on the TMJ and associated pains, to whom he/she can refer you.
The attempt I have made in this chapter is just the start of your studies, if you are suffering from such pains. This material has been based on what I learned in school and from my experience in practice, but there are many people who know more and have written about each subject in other locations on the internet. Be sure to expand your studies of these difficult subjects with any other sources of reliable information you can find!