If you would like to explore more details on dental decay and tooth infection and consequences you may want to check with the Wikipedia page on this subject. They provide ample references to the literature and links to supporting information.
Organization of This Chapter
You may Skip to Whatever Subject Interests You Now
Basics
The Nature of Decay
The Detection of Decay
Sites of Decay
Occlusal (Biting Surface) Decay
Proximal Surfaces (touching adjacent teeth)
Facial and Lingual Surfaces
Decay of Roots
Deep Decay and Symptoms
Treatment Options
Fluoride
Bottom Line for Infection: Decay
…………………………………………………………………………………………………………………………..
Basics
Now it’s time to leave the theoretical and idealized considerations of the last section and look in more detail at real things that happen to real teeth. Everyone knows about “cavities” and the need for fillings, but do you really know what causes these problems, and what happens if the decay goes too deep toward the pulp, or undermines too much of the tooth? Do you know about the different kinds of cavities that people get at different ages? What are the symptoms of decay? And, importantly, how does one prevent decay?
It is crucial to realize that decay happens because there are specific bacteria in the mouth that stick to teeth and, when given the appropriate nourishment, make acids. Even enamel, as hard as it is, is susceptible to the acids made by these bacteria. You are no doubt aware that there are acids that attack concrete, and even glass. But it takes no such powerful acid to attack the tooth structures. The acids made in the mouth by these microorganisms are similar to vinegar, but when localized near one site on the tooth for a long enough time, they can leach the mineral out of the enamel or dentin.
People who like to eat lemons (yes, there really are some) can demonstrate very clearly that citric acids is strong enough to dissolve enamel. Often these people lose most of the enamel on the facial surface of the teeth that are most in contact with the acid, principally the upper incisors. Bolemics, who commonly induce regurgitation of their meals, are found to have eroded the lingual surfaces of their teeth due to the adverse effects of stomach acid!
The difference between the lemon enthusiast or bolemic and the bacterial decay situation is that the bacteria focus the acid attack on a particular spot on the tooth, and when that spot becomes soft, they invade the tooth structure. This invasion eventually causes the tooth to be destroyed from the inside out, as opposed to the other erosive processes that go from the outside in.
The Nature of Dental Decay and Tooth Infection
Dental decay and tooth infection has been with us for a long time, and probably will stay with us into the distant future. The bacteria that cause decay are ubiquitous in the environment, but strangely enough, must be initially transferred to the newborn infant, most likely from the mother. Some people harbor much higher levels of decay-causing bacteria than others. This is likely due to several factors, including the amount of sugar and starches in the mouth for the bacteria to eat, how many surfaces there are in the mouth where the bacteria can hide, and how effective the body is at fighting off the bacteria using the components of the saliva.
The presence of decay really marks a removal of mineral from the surface of the tooth. This leaching out of mineral will eventually produce a soft, penetrable layer that must be removed and replaced with a suitable artificial material (a filling). But some REmineralization can take place before the surface irreparably breaks down. If the beginning of this process is detected early enough, the body can sometimes remineralize the area. This remineralization is due to the presence of calcium and phosphate in the saliva – these are the major components of tooth mineral.
The presence of bacterial can prevent the body from remineralizing decaying areas, but the saliva also contains antibodies that specifically attack these bacteria. So, the salivary glands are actually very well designed to control the decay process. So why do we still get decay? It is because we manage to defeat the best efforts of this natural system with our poor oral habits!
I’ll try not to moralize, but if our oral bacteria were pets, they would probably feel better cared for than our cats and dogs! Why is it that the food that appeals most to us also appeals to them? Also, notice that we and they can eat it at the same time ….
You may have heard about the two villages in rural India …. (Actually, there have been pairs of villages like this in many parts of the world). As the story goes, everyone in the two villages was very happily going about their village-type activities, when someone built a train line near one and put in a quick stop. This stop was apparently just long enough to offload this new brown fizzy stuff that came in a neat glass bottle. So sweet and refreshing! Well, the two villages didn’t have much communication with each other, and the more “modern” of the two wasn’t about to share its resources of cola. Visitors to the villages, medical and dental missionaries for the most part, noticed that within a few years the primary health problem in the cola village was tooth decay! This problem had been very rare previously, and was still rare in the more remote of the two villages. The severe tooth pain that was increasingly experienced by children near the train tracks was perhaps a high price to pay for one benefit of modern industrialized society.
Now, it is possible that a fair amount of the decay experience with colas is due to the acidic content, although carbonic acid is very weak. But the sugar content is an obvious culprit. I had a patient once that had so much decay on the outer surfaces of his teeth that I thought he had been addicted to methamphetamine, or had had head and neck radiation treatment. The picture below is similar to what I saw in his mouth.

When I asked him about what could be causing this problem and asked about drug habits, he replied that he drank a lot of coke. How much, I inquired? About FIVE 1 1/2 litre bottles per day!
We can so easily override the decay-fighting abilities of the body – but can we enhance these abilities in some way? Later we will see that one particular treatment not only helps to kill bacteria, but also makes the tooth structure harder and helps in the remineralization of the tooth. What is this treatment? Fluoride!
There are four factors that most influence the tendency to have decay: bacteria, presence of food, flow and composition of saliva, and presence of minerals and fluoride. All four of these must be considered together in order to predict how much of a problem you will have with decay. Note also that all four of these factors can be influenced by genetics, race, age, and of course behavior.
So now that we have a feeling for how decay happens, how does the dentist figure out how much of a problem you have?
Detection of Decay
In principle there are just two ways to detect dental decay and tooth infection. Finding it with a dental explorer (that sharp pick that you hope doesn’t stick when the dentist pokes it into the grooves of your teeth), and seeing it in a dental X-ray.
The dental explorer has many different forms, but a picture of several types is shown below. The common feature is a sharp point. It is this point that can penetrate into the tooth if the surface is soft. The resistance to removal of the explorer once stuck in the tooth surface gives a little tug and “boing” that strikes fear in the hearts of the bravest patients. And believe me, it makes the dentist feel bad also. This is especially true when he/she finds a spot like this in an area of the tooth that is either extremely difficult to get to, or impossible.

The dentist will typically check several key areas of the tooth for decay, particularly in the occlusal grooves on the biting surface of the tooth, and any other grooves or pits and fissures. Sometimes the groove in the tooth is just the right size to catch the point of the explorer, but there really isn’t any decay there. Typically this kind of deep groove in many people is just the kind of place that bacteria like to hang out, and eventually decay will start. Sometimes the dentist will choose to place a SEALANT in this area, which is just a plastic coating to fill in the groove, but a filling doesn’t need to be done unless there are additional signs of decay. These additional signs might be demineralization in the form of a whitish or chalky appearance seen around the edges of the groove, suggesting that decay is affecting the enamel or undermining the enamel by leaching out the dentin underneath. Alternatively, the dentist may feel that there is a soft bottom to the groove, also implying active decay.
So the dentist relies on the feel of the exploror in areas where decay is likely, and on the appearance of the area as well. In some areas that can’t be readily seen, but where there is access by the explorer, feeling will have to do (root areas between teeth or between roots of one tooth, for example). But, what about areas that can’t be seen, and where the explorer won’t reach? Here we must depend on X-rays.
Dental X-rays are shadow pictures using invisible light. This light penetrates the soft tissue and reveals a great amount of detail in the hard tissues. For example, the dentist can differentiate easily betwen bone, tooth root, tooth enamel, dentin and any filling materials that might exist. Even the passages in the bone through which the nerves pass can be seen clearly in many instances. The value of X-rays in dental diagnosis cannot be overstated – this technique plays an absolutely pivotal role in the dentist’s ability to plan his/her treatments.
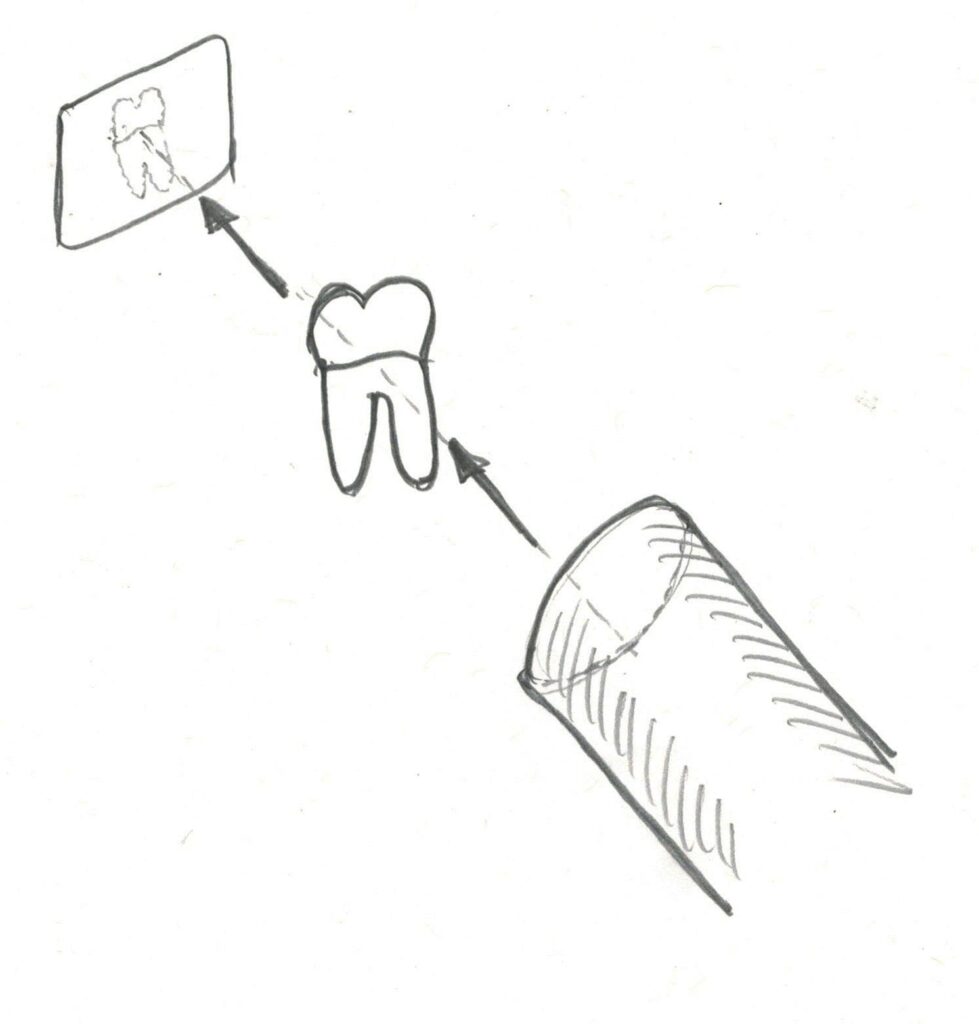
Again, let us look at the geometry of the shadow picture as it relates to dental X-rays. The following diagram shows the light source, the tooth and the film. As the positions of the light and film are changed relative to the tooth, then the image of the tooth will vary. It is the skill of the dentist or assistant that allows even individual roots of a tooth to be seen clearly enough to be able to tell, for example, how close to the apex of the root the filling material went in a root canal treatment.
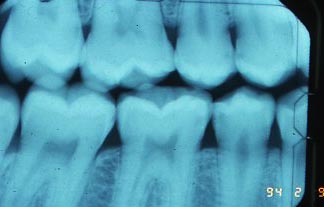
The dentist can detect decay easily using this technique. The following photograph shows X-ray images of several teeth. On the left side you can see what the healthy tooth should look like. The whiter area round the periphery of the crown of the tooth is enamel. It is whiter because it is more dense and blocks more of the X-rays. (Note that film becomes darker when more light hits it. This reversal is why it is called a negative, in photographic terms. In dentistry and medicine, however, no positive or print is ever made.) The darker areas inside the tooth are the pulp chamber and root canal system. There are only nerves, blood vessels, lymph ducts, cells and fibers in these areas, so nothing stops the light, so the light through here darkens the film. You can also see the bone level around the tooth.

Toward the right side of the picture on the bottom near the area where a tooth is missing, you see a tooth which is clearly missing a lot of structure on the proximal surface (contacting an adjacent tooth). In this case it is likely that there is significant decay in the area. It is also possible that some of the tooth structure has broken away. Sometimes visual observation is required to get the whole story. It appears darker because the demineralization has made the area more transparent to X-rays, or that there is less tooth structure there. Note that X-rays help with detection of decay on surfaces that are oriented parallel to the light beam. Thus, the proximal surfaces of the tooth are easy to see. This is great, since the dentist cannot easily feel these areas with his explorer. But, the facial and lingual surfaces of the tooth are superimposed in the film on the body of the tooth, making it more difficult to distinguish subtle changes in density. The occlusal surface, even though it is oriented ideally, is so convoluted that the junction between the dentin and enamel cannot be visualized clearly here. So occlusal decay has to be really deep to be distinguished clearly on the X-ray film, and earlier detection is always possible using an explorer.
In case you are wondering, the pure white areas of the X-ray above are showing amalgam fillings – where the metal is dense enough to block ALL of the X-ray beam, so none exposes the film in that area.
A combination of techniques: exploration, inspection and X-ray imaging will allow us to find virtually all areas of decay on the teeth. Small, incipient areas of decay may be missed at one visit, but should never be missed when it is large enough to require restoration.
Exceptions? Sometimes decay begins at the edge of a restoration (crown or filling). It can be very difficult to notice where the invasion occurs because rampant decay of the tooth is deep inside where it cannot be visualized. And X-rays are also blind in these areas since the filling material or crown often completely blocks the X-rays. In general it is rare that any significant decay will be missed.
Sites of Dental Decay and Tooth Infection
There are four main sites of tooth decay, the biting or occlusal surface, the proximal surfaces between adjacent teeth, the facial/lingual surfaces and the root surfaces. We will look at each area in more detail.
Occlusal Decay:
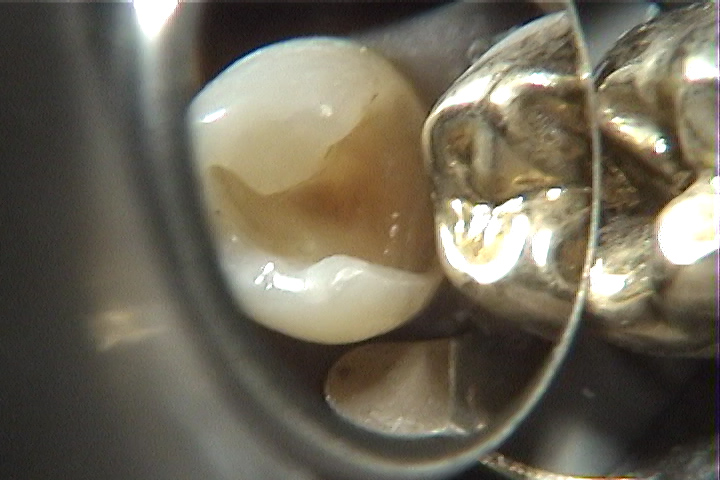
The photographs below show two extreme situations that are encountered. First there is an upper premolar with some staining in the grooves toward the canine contact, but no indication of demineralization. In the second picture the decay has clearly undermined much of the tooth structure (some was already removed by the dentist using a bur, but this decay is still reaching farther down into the tooth). The enamel and dentin in this area have been broken away by the action of eating or brushing, revealing the interior of the tooth. In this situation the bacterial invasion may very well have penetrated to the pulp – the living portion of the tooth.


Decay of proximal surfaces, contacting adjacent teeth:
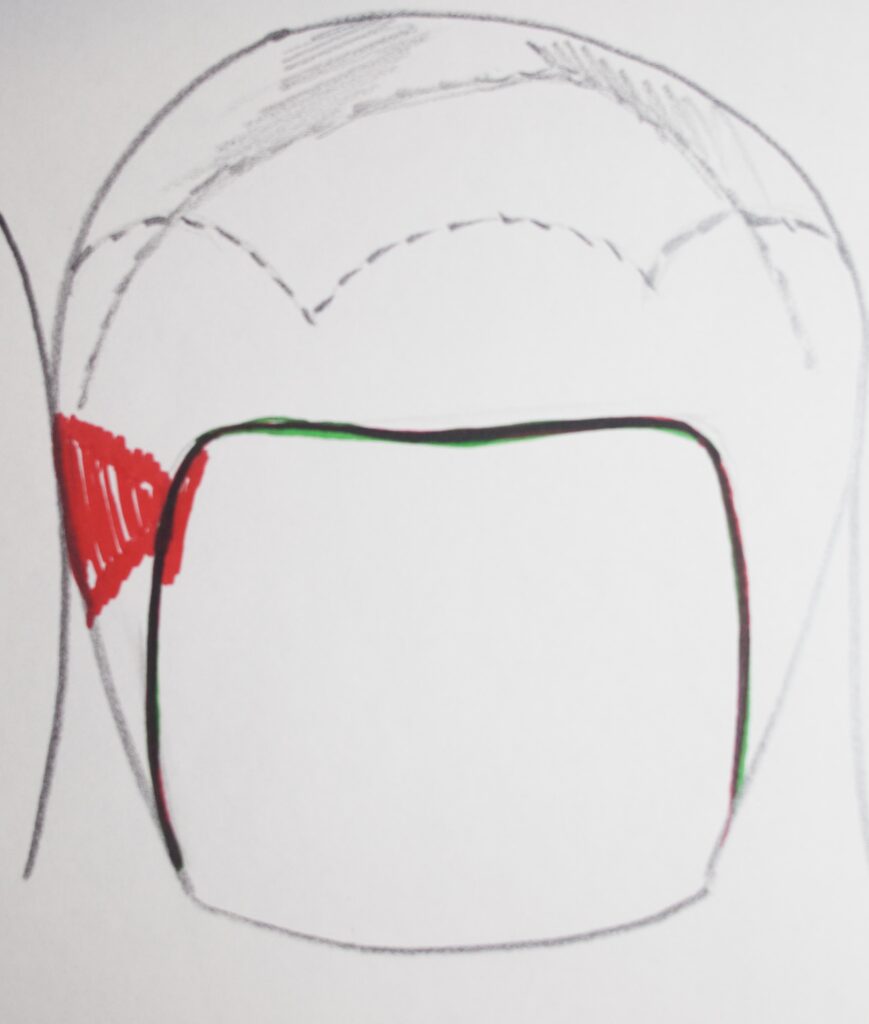
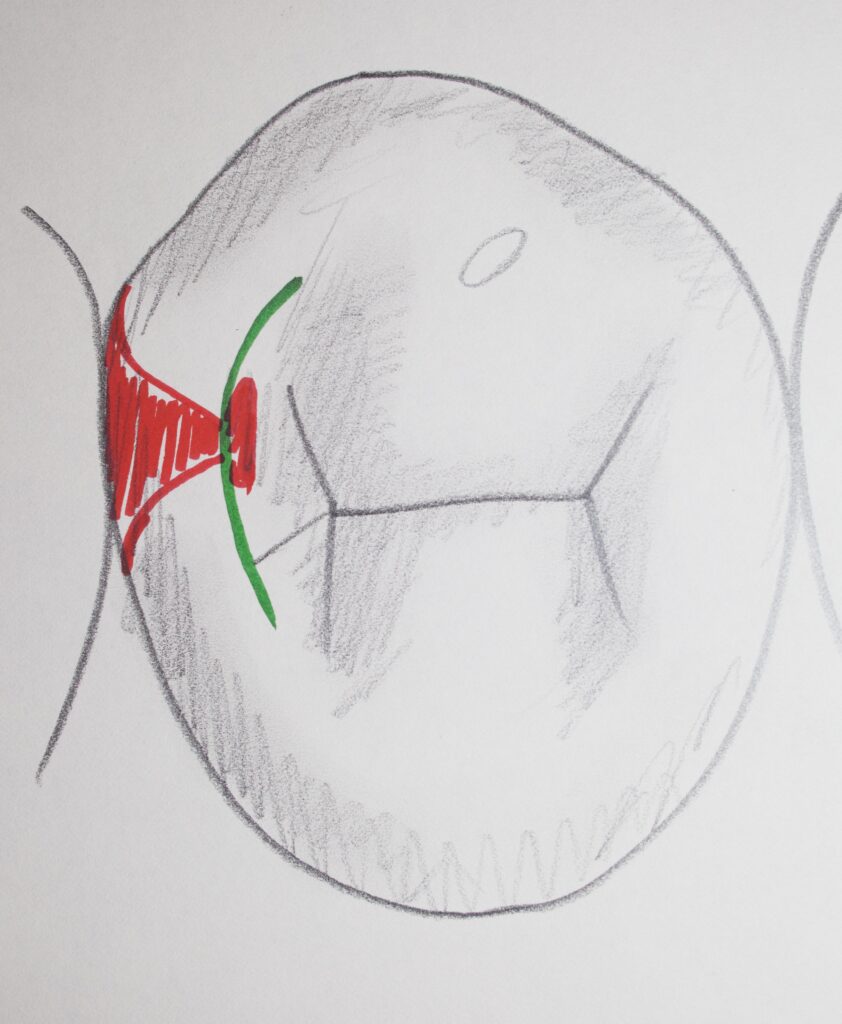
Below are two drawings showing what the decay pattern looks like for the proximal surfaces of teeth, typically. You can see how the red decay tends to spread out when it hits the dentin at the dentino-enamel junction.
Decay problems on the occlusal surfaces happen earlier in life, and the proximal surfaces tend to decay starting in the late teenage years. Note in the X-ray picture below the decay on the proximal surface, minimal and moderate. The darker shadow of decay has just barely reached the junction between the dentin and enamel in several areas. The little dark area in the dentin just inside the enamel is the tell-tale sign. These teeth will have to be restored because of dentin involvement.
More will be discussed about X-rays in Chapter IV.3, but for now, any darker area in the film of the tooth indicates a loss of tooth structure, or a loss of mineralization in the structure.
In the pictures below, this is a situation where the tooth is being prepared for an amalgam restoration, and in the process the decay INSIDE the tooth is very obvious. In the box form on the side toward the canine, there is a whitish area, which is decalcified enamel, and there is a darker, soft area where the dentin is involved. Several of the teeth in the first X-ray above would probably look just like this on the inside.
In the second picture below, a partially prepared tooth shows how some decay is still migrating along the DEJ (junction between the dentin and enamel), when there is little or no whitish decalcification showing in the enamel where it has already been removed.


The photograph below shows how decay appears on the proximal surfaces of front teeth. Since the tooth is thin and the light can shine through it readily, we can often see the same signs of decay migrating along the dentin by observing with a good light behind the tooth. You can actually see the DEJ through the tooth structure as well.

Decay of the Facial/Lingual Surfaces
The picture below shows rampant decay on the facial surfaces of these front (anterior) teeth. There will be the need to excavate that decay with a rotating bur, followed by a large restoration with something tooth-colored.

Decay of the Roots:
This X-ray shows clear root decay on both of the adjacent premolars in the area marked “E”. You can see where the enamel and dentin meet at the surface of the teeth, and a clear shadow extending into each tooth at this area. For the second premolar it is approaching the pulp chamber more closely, but not likely to have resulted in an exposure yet – so no root canal needed.

The left side of the X-ray demonstrates decay starting in the root area of the molar. This decay pattern is much larger and seems to be just at the pulp chamber. Whether a root canal is needed must be determined by excavating all of the decay to see if there IS any sound dentin protecting the pulp. The next section, discussing deeper decay, may well be illustrated by the X-ray above.
Deep Decay and Symptoms
In the situation illustrated above, where decay encroaches on the pulp or canal system of the tooth, pain can certainly result. This is what suddenly alerts you to the problem. This is also where most people really blow it. That first tinge of pain says, “oops, there is something wrong with my tooth! If I brush a lot for a couple of days it will clear up. The last thing I want to do is go to the dentist, that will REALLY hurt”! Sometimes people even put an aspirin tablet against the gingiva near the painful tooth – that seems to help the pain, but the problem is made no better, and they will get an aspirin burn.
Now, of course, you’re out of the frying pan and into the fire. You will endure bravely a severe pain to avoid going to the dentist where you can (really) expect minor pain at most. In the process the seriousness of the situation steadily worsens and the cost and time and effort to effect the repair increase dramatically.

So, what kinds of pain might be signals that deep decay is going on ? The first you will notice is sensitivity to cold. Take a big gulp of ice-cold soda and then move your tongue so it swishes past all of your teeth before it has a chance to warm up. If you are anything like me and most other people, just thinking about it will send shivers down your spine. You are already avoiding cold on certain teeth, aren’t you? The good news is that you can have sensitivity to cold for several reasons and decay might not be involved. If you have exposed dentin due to wear, it is often sensitive to cold. If you have exposed dentin due to gum recession if may be sensitive to cold. So, don’t panic yet!
On the other hand, what if you are sensitive to sweet foods? This MAY indicate decay, but also could be caused by other exposed dentin surfaces.
Sensitivity to hot could suggest more of a problem. Most of the time this is a signal that a decay process has started and that it is approaching the pulp.
The big one is LINGERING PAIN. If cold sets the tooth off and the pain lasts for more than a few seconds, then you have a problem. The cure may be simple, but the longer the pain lasts the more of a problem you have. THROBBING pain is a clear sign that the nerve is fully involved and probably that the infection has gone down the canal system into the bone as well. Of course, most people at this point are on the phone to the dentist, ANY dentist, but sooner would have been nice.
Is it possible that the decay can have gotten to the pulp and yet there is no particular pain sensation? Yes. If the decay process is slow then for some people the pulp can die, and the nerves along with it, and no one will be the wiser. This does not mean that the tooth doesn’t need to be fixed. The pulp is still infected and when the infection reaches the bone some serious pain can start. This can occur at the most inconvenient times – a business trip to Russia, during the last week of pregnancy, the night before a major sales presentation or final exam ….
If there is a suspicion that the pulp is dead and yet there are no symptoms to speak of, then often an electric pulp test is done. An increasing but small current of electricity is passed through the tooth. If you don’t feel anything at any level of current, but you do in the other teeth tested, then the pulp is probably dead and the tooth must be treated.
Let us look one step further in the decay process. The X-ray below shows how the really massive infection of the crown of the tooth has passed down the root canal system into the bone. The dark area around each of the root apices represents a demineralization of the bone due to the infection, just as we have seen for the tooth structure.

Bone infection like this might be pain free, but most often is not. It has a lot to do with the pressure that builds up in these areas. What is building up this pressure? OK, we’ll use the dreaded word. Your dentist or physician will call it exudate, but the rest of us call it PUS. Doesn’t that conjure up nice images! The fact of the matter is that infections generally produce a lot of dead cells and this debris needs a place to go, to DRAIN. In the case of a really big infection down the root canal, the drainage may go back up the tooth. That relieves the pressure and thus also the symptoms. Sometimes these ABSCESSES drain through the bone itself into the gum tissue, and then through it was well into the mouth. The taste is not great, but the pain is relieved.
We’ll see more about problems in the bone in a later chapter, but for now it is important to realize that this kind of a problem is a direct result of decay, that is an infection of the tooth that spreads every way it can. You must be aware of the potential seriousness of these kinds of infections, because in some individuals with infection in some location, the infection can be possibly life-threatening if spread to the wrong area.
Treatment Options
Treatment of decay depends on the extent of decay. As can be surmised from the discussion above, this can range from simple application of fluoride on a regular basis, to a lengthy hospital stay.
Please don’t dwell on this distressing thought any longer. Let us review briefly some of the more common treatment options, although most will be described in more detail in later chapters.
First, a truly incipient decay area can often go away with an increase in the amount of topical fluoride (applied directly) and a decrease in the amount of sugar. Remember our model for decay, there is a balance of factors which either cause net demineralization or remineralization. If we can influence that balance in the right direction then the process can be reversed, as long as the decay has not broken down the structure of the enamel surface, nor has invaded the dentin layer.
I was talking with a dentist once who related an experience he had while preparing to take the Board Exam for state licensure. In these exams the dentist is required to treat a patient with interproximal decay by placing a silver amalgam filling. Naturally, the closer to idea the higher the grade. If the decay is too deep then the filling can’t be “ideal”, meaning minimal. So Board candidates find patients who have incipient lesions that have JUST reached the dentin. This particular candidate had found a patient 4 months earlier who had a nearly perfect lesion (place of decay). It was not clear that it had really reached the dentin, but he figured it would be starting to move rather quickly through the dentin at any time. To play it safe he put the patient on fluoride a couple times a week to keep the lesion from getting too deep. Taking another X-ray two weeks before the exam he found that the lesion was GONE! This certainly represented a valuable object lesson to the dentist, and should to us as well.
Decay that has clearly advanced to the dentin must be removed with dental instruments (drills and scrapers) and then the area that is left filled with some material or combination of materials. Later chapters will discuss various options here. Visit Chapter V.2 – for examples of fillings for posterior teeth.
If the decay threatens the pulp but there is still some hard dentin left covering the pulp, again a simple filling is required, but it may be wise to place something over the area closest to the pulp that will stimulate the cells in the pulp to make more dentin in this area.
Even if there are signs of decay right at the pulp, it is often found that stimulation of the pulpal cells can cause more dentin to form which walls off the decay process and that the pulp will heal. This pulp capping technique is sometimes effective and adds years to the life of the pulp, but there are some who claim it is doomed from the beginning and a root canal treatment should be done.
Root canal treatment is done when the decay is too advanced toward the pulp. But there are also times that the decay is so advanced down the side of the tooth that a simple filling is not possible. In these instances the filling would have to be placed too close to the bone and the gum attachment to the tooth disrupted. The procedure required here is to lower the level of bone in the area so that the filling can be placed sufficiently far from it. This crown lengthening procedure may involve just the removal of excess gum tissue, but often requires bone recontouring.
If the decay has removed too much of the dentin in the crown of the tooth, then it is possible that there is no dentin support for much of the remaining enamel. We will talk about design of fillings later, but for now it is sufficient to note that when too little sound tooth structure is left one can often not safely place a simple filling. There may be precious little to fill, but also that which is left may not be supported by the filling material. In these cases it is often necessary to make a piece of cast gold or other metal or even porcelain which covers and protects the remaining tooth substance. These artificial crowns or onlays are often required even though root canal therapy and crown lengthening procedures are not.
And again, in the extreme case where the tooth cannot be restored then it must be extracted and the space filled by a reasonable substitute in order to maintain the bite geometry and function. The substitutes may be removable partial dentures, bridges or implants, all of which shall be discussed later in this site. Visit particularly Chapter V.13 for discussions of tooth replacement.
Fluoride
As we approach the end of this chapter, there doesn’t seem to be a better place to discuss some issues with respect to the use of fluoride. The first community to put fluoride in their drinking water was Grand Rapids, Michigan in 1945. This wasn’t really such a monumental experiment as one might imagine, for many communities with fluoride in their water had been studied extensively, it’s just that this fluoride was natural. These naturally fluoridated communities were known for their remarkable lack of dental decay, and over the course of the next 15 years a dramatic decline in the decay rates in Grand Rapids was noted as well. Today, the great majority of the communities in the U.S. have fluoridated drinking water, and the levels are adjusted carefully.
However, one must realize that too much fluoride can cause a chalky or stained appearance to the teeth, which is termed fluorosis. This does not normally show up until the levels are 6 – 8 times the desired one part per million of fluoride in water, but one must be careful not to overdo it. In particular, consider that there are several other sources of systemic fluoride. Physicians often prescribe flouride tablets for infants and kids before the dentist ever sees them. If the water level in your community is already high enough then this may be excessive. Also, if your child is in the habit of swallowing toothpaste, this can add substantially as well. It is best to check with your water company and dentist in order to make sure that your child is not getting too much fluoride.
While the flouride that is consumed systemically is responsible for hardening the structure of developing teeth, the application of TOPICAL fluoride, as described earlier, is also very effective in many ways. This topical application is of great value independent of age, and often special trays to hold fluoride are made for patients late in their adult and senior years!
One final note – it was at one time espoused by some that the use of fluoride in drinking water was a COMMUNIST PLOT! The people who said this are part of a group commonly termed antifluoridationists. The reaction of these people to fluoride use was to some extent motivated by the feeling that the government was doing something to everyone, taking away personal freedoms. Another motivation came later when a couple of biochemists reported risk. In the decades following these struggles it has been shown many times that the biochemists’ conclusions were wrong, and that all subsequent data confirms the safety of fluoride. Also the communist plot theory doesn’t get much attention anymore – although it does bear a certain resemblance to Russian hacking ….
Bottom Line for Infection: Decay
Decay-causing bacteria can be harbored in many places in the mouth, and these places are more accessible at different ages.
Certainly, keeping the plaque removed from the teeth on a frequent basis, and making sure that the fluoride concentration around the teeth is sufficient to form more decay-resistent enamel, are the best preventive measures that we can take at this point in time.
Once the decay has penetrated through the enamel to the dentin, it is time to remove tooth structure and the decay and restore the tooth with some artificial material – a filling.
If the decay has progressed very far, it may be exposing the pulp, requiring root canal therapy. But, even if the pulp has not been exposed, at least a very large filling must be done, and possibly a crown.
It is very much to our advantage to keep the bacterial plaque off of tooth surfaces regularly – otherwise we may be putting a lot of unexpected charges on our credit cards!