For another resource on Gum or Periodontal disease you may wish to explore the website of the American Academy of Periodontology.
Organization of this Chapter:
You May Skip to Whatever Subject Interests You Now
Introduction
Periodontal Health Provider
Nature of Gum Disease
Monitoring of Gum Disease
Diagnosis of Gum Disease
Sites of Periodontal Infection
Treatment Options
Prevention/Home Care
Bottom Line
………………………………………………………………………………………………………………………..
Introduction
This chapter deals with a potentially hazardous subject (I avoided the word touchy). While the condition of the gum tissues (gingiva particularly) is the prime consideration, there are other agendas, even political ones that come into play here.
Consider that there are three dental professionals in the treatment arena that may help you with gum disease, including the diagnosis of the disease and its management. These are the general dentist, the periodontal specialist and the dental hygienist. We’ll look more closely at each of these people soon, but you need to know that there is something of a TURF BATTLE going on between dentists and hygienists, the later of which would like the option to practice independently. So far patient treatment has not been compromised due to this political contest between representing organizations, but you should be aware of the issue.
Another issue relates to the proper management of patients with gum disease. Sometimes the dentist or hygienist may not adequately diagnose the disease and fail to treat or refer as appropriate. This is not generally noticed by the patient because gum disease (gingivitis and periodontitis) are INCIDIOUS diseases. That is to say the patient often has no symptoms that prompt treatment – but wait too long and tooth loss can ultimately result. Tooth loss due to periodontal infection is becoming more common than tooth loss due to decay.
Before describing the details of the disease, we’ll look more closely at the “playing field” in the periodontal arena. I don’t want to give the idea that the field is particularly contentious, but it may perhaps be said that the level of care of patients with periodontitis runs the gamut from undertreatment to overtreatment, and the more you know about the environment of treatment, the more you can be assured of the appropriate level of treatment.
The Periodontal Health Provider
The general dentist, if graduated from school rather recently, has extensive training in periodontal disease (more commonly known as gum disease of pyorhea) diagnosis and management. Alternatively, older graduates have wide options of continuing education courses available to learn about periodontitis management. Most states require a dentist to pass a board exam for licensure that requires diagnosis and/or initial treatment of a patient with this disease, but this wasn’t always the case. The dentist will generally know what is going on, and hopefully apply this knowledge thoroughly to all of his patients. The average dentist realizes that failure to diagnose and treat this disease can potentially jeopardize the patient’s oral condition in a very serious way. Still, due to lack of education, lack of interest, or in some cases lack of communication, patients DO sometimes get through dental offices without being well counseled on the condition of their gingiva. We shall try to see that this does not happen to YOU.
When the general dentist detects gum disease in a patient the choice for treatment is to either do it in his office, refer the patient to a specialist (periodontist), or to ignore the situation. In the great majority of cases only options 1 or 2 are utilized! The periodontist is trained to perform treatment procedures in which most general dentists have little experience. This is not to say that a general dentist may not, when adequately confident, perform such procedures, but mostly they are left to the specialist. These techniques include surgical management of periodontal disease, cosmetic correction of gum tissues (plastic surgery of the gum tissues), and even placement of implants. The periodontist does a lot of non-surgical treatment, which is well within the boundaries of a typical dental office, but the specialist’s main interest is in the more sophisticated techniques. The typical fees in a periodontists office will be higher than for the same procedure done by a general dentist, due to the extra years of training to become a board-certified periodontist.
Now, both the licensed periodontist and general dentist frequently employ dental hygienists. Since this is traditionally, but not exclusively, a position filled by women, we will use the pronoun “she” where appropriate. The hygienist is specifically trained in the diagnosis, non-surgical management or periodontal disease , and in the instruction of the patient in appropriate home care techniques. As an employee, she must follow the guidelines laid down by the practice owner, but generally they are given a lot of autonomy. They manage their own instruments and supplies, for example, and can direct and evaluate the treatment of their patients. In some states, however, they are not allowed to administer local anesthetic, and the nature of their work is such that it must fit within the context of comprehensive dental treatment. The hygienist is not trained in the detection and management of decay and other dental problems. Her field of expertise is soft-tissue management and as such she may not advise patients beyond the rather limited bounds of her educational background and licensure.
After we have studied the nature, progress and treatment of periodontal diseases in the next few pages, we will return to the issue of appropriateness of treatment in specific instances. We will look at how the dental professionals described above should act in concert to see that the patient receives no more nor less than the treatment necessary.
The Nature of Gum Diseases
Recall that the term gingiva describes the part of the gum tissue which covers and attaches to the bone and teeth. Look in your mouth (use a mirror), and see where the gingiva is for the lower incisors. Note there is a line where the tissue becomes moveable (pinch your lower lip and slide it back and forth). The loose stuff is called mucosa, but everything that is fixed (and generally pinker) is the gingiva. It extends all the way up to the tooth surface, and is connected with it. Now any disease, infection or disorder that affects the gingiva may be termed gum disease, but we shall have to specify the different types more closely.
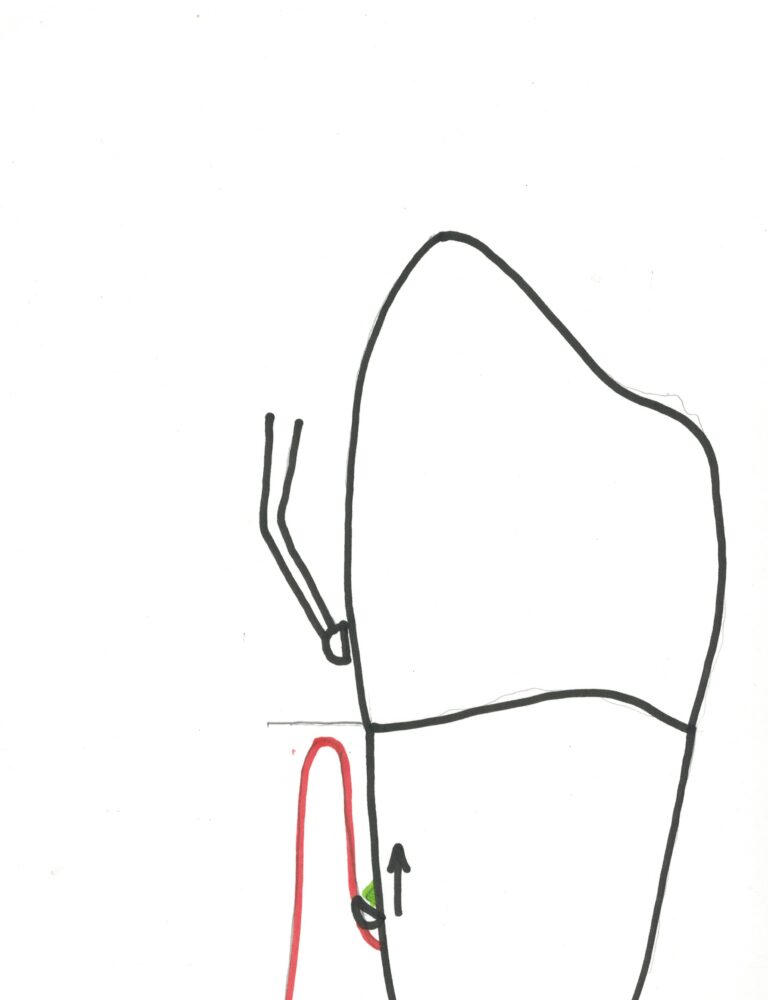
The simplest and most common gum disease is gingivitis. Anyone who watches any television at all will have heard of this. It is a simple infection of the gingiva, and really involves only the FREE GINGIVA. (Now may be a good time to visit Chapter II.3 and Chapter IV.4 and review some concepts related to the soft tissue support of the teeth). The sketch below shows the areas that are involved in gingivitis and in periodontitis. The area of (red) gingiva where the probe has been inserted is FREE in that it is not attached to the tooth. The LEVEL of attachment in this case is on the root and it is said there is attachment LOSS since it is no longer on the enamel.
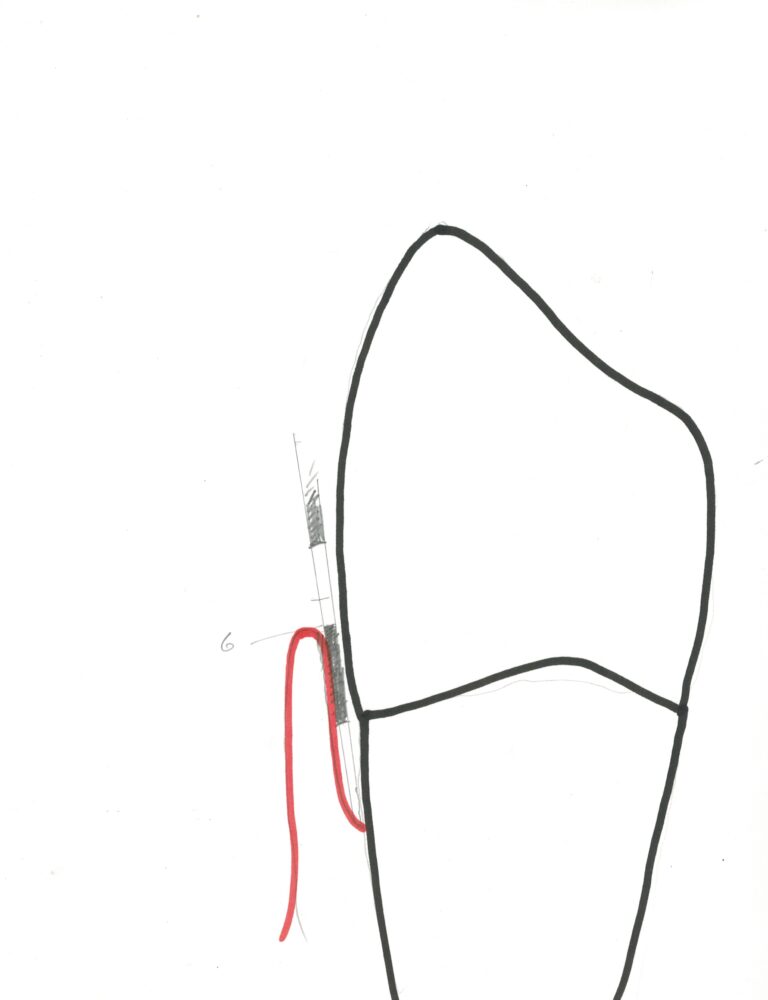
If you have gingivitis alone, you have an infection of the free gingiva but no loss of attachment to the tooth, and no loss of bone support for the tooth. If you have periodontitis, by definition, you have lost attachment and bone level, and have an active infection.
We’d better consider what infection means. Typically, when you have gingivitis your gums between and covering the facial surfaces of the teeth are swollen, red, tender and bleed with slight provocation. In other words, your gums are an EYE SORE. We tend to see a lot of gingivitis in kids whose parents don’t seem to care whether they brush or not, or allow them to brush unassisted and unobserved. It is really a shame to see a teenager who otherwise looks fine, which is no mean trick during adolescence, with bright red gums which are puffy and loose around the teeth.
So what causes this infection? Like any infection, it is the presence of foreign material in the body. When you get a splinter in your skin and don’t take it out, what happens? First, it gets red, then tender, then swells up and gets really tender and if you’re lucky the splinter will soon slide out on a sea of pus. If you’re not so lucky, the discomfort will soon have you digging it out when the tissue is extremely tender to the touch and you must endure maximum pain. Exactly the same thing happens in the gum tissue!
The foreign bodies that infect the gingiva are bacteria and their products. What kind of bacteria? While some are similar to those that can cause tooth decay, there are dozens or hundreds to choose from and they are in the mouth all the time. But when you allow them to sit in the SULCUS or pocket between the free gingiva and the tooth for any length of time, it’s just like the splinter. A battle will be engaged between the bacteria, which are invading the body through the sulcus, and the immune cells of the free gingival tissue. When the body attempts to fight off invasion, the affected area is flooded with immune system cells that like to eat foreign objects (these immune cells are pushed out of the capillaries in the area from the blood stream, and the fluid that accompanies them causes the area to swell up). Dilation of the blood vessels in the area increases the amount of blood locally and gives rise to the color. During the battle there are chemical messages sent back and forth from the front line troops (immune cells) and the troop ships (blood vessels) communicating the status of the attack and resistance. Some of these chemicals produced have the effect of stimulating the nerve endings in the area, just to make sure that you know there are hundreds of thousands of little unicellular foot soldiers giving their all to protect you from invading forces.
The analogy above can be seen to represent very well the battle that goes on in your gingiva if you allow the invading bacteria to get a foothold. As the bacteria gain a foothold, staying in one place long enough, they build bulwarks, to protect themselves. These “bulwarks” are really TARTAR, or more professionally, calculus. Calculus is a mineral deposit made by the bacteria, which sticks to the tooth surface and gives the bacteria a safe haven in which they can multiply and send foray after foray in the assault on your gums. If you don’t get in there and physically remove the calculus from the teeth, then you will loose the battle.
Calculus (tartar) is a strong irritant to the tissues, not because of the mineral content, but because it is filled with bacteria! When you get a splinter in your skin it’s the bacteria that are on it that cause the swelling and redness and pain. Step on a nail and everybody knows that you must get a tetanus shot. Why? Tetanus is an example of a bacterium which is common but does not flourish in the presence of air. If it can penetrate deep into your body where there is no free air, then it can multiply and produce toxins which can cause you great trouble indeed! These bacteria actually produce poison inside your body. And yet, if you surgically implanted a sterile nail in your body it wouldn’t cause you that much of a problem. (By the way, a tetanus shot works by stimulating the body to produce SPECIFIC immune cells which attack tetanus bacteria so the body doesn’t have to wait and figure out which soldiers are most effective by trial and error).

So, you’ve got calculus in the gingival sulcus and bacteria from it are attacking the free gingiva. This battle is taking place close enough to the surface so that free air (oxygen) is available, and the bacteria in gingivitis are all air stable (aerobic). These are the least harmful bacteria, so gingivitis is not life threatening and does not, in itself, cause any irreversible damage. If you have not lost any attachment then you can have the calculus cleaned out and eventually, with good home care (brushing and flossing) you can get the gums back to their normal pink and strong condition, and again have that movie-star smile.

Before proceeding to discuss what happens if anaerobic bacteria start to colonize in these areas, I can’t resist yet another analogy for calculus. For those of you who have spent any time at coastal beaches where there are harbors and piers, you will have noticed that where these pilings (and even boats) are submerged frequently under water, there are lots of BARNACLES. Barnacles are little teepee-like shells which adhere very well to the piling surface, and inside there is a little animal. This animal made the shell immediately after he got a foothold on the surface of the piling. Once the shell is made the animal is immune from attack and can live out his life in blissful safety.
When bacteria first start to attach to your tooth surface they form a kind of gooey coating called PLAQUE (here’s another popular advertising term). Now it doesn’t take more than a little effort with a brush or floss to remove plaque every day, but once it has made its calculus shell (by mineralization, just like the barnacle), you can’t brush it off! Think of your teeth as a bunch of pilings in a sea of gingiva and you’ve got the picture.
Now, lets get back to the possibility of anaerobic bacteria in the gum tissues. We said that these bacteria can’t live in the presence of free air, and that they can make some pretty nasty toxins. Well, no one really knows just how they get a foothold initially, but when they do get established the toxins cause loss of gingival attachment, formation of deep periodontal pockets, the depths of which have no free air present, loss of bone support for the teeth, and an inflammatory response. Now you are officially the proud owner of a case of periodontitis. This is the kind of infection which will cause gum recession and ultimate loss of teeth.
Simple gingivitis does not, in and of itself, lead to periodontitis. One can speculate, perhaps, that when calculus builds up enough to block access of air to the gingival sulcus, the anaerobic bacteria can colonize and initiate pocket formation. Then, even if the calculus is removed later, the anaerobic bacteria can still colonize easily in the depths of the deeper pockets that have now formed and initiate more destruction.
How does one get rid of the anaerobic bacteria from the periodontal pockets? First, certainly don’t let them build up calculus down there, and if they do make sure you get it removed. Second, try to maintain the surface of the tooth as smooth as possible to try to keep more calculus from adhering. Third, since YOU cannot effectively clean bacteria our of these areas due to the deep pockets, keep the general environment as clean as possible, and avoid any superficial gingival infection that can cause swelling and make the pocket even deeper.
Note that you can have attachment loss due to periodontitis, but NOT have an active gingival infection with tender gums and bleeding. You have a HISTORY of periodontal infection, which predisposes toward further problems, but currently have healthy tissues.
Later, We’ll see more clearly the treatments necessary to fight off periodontitis and stabilize the attachment complex to further loss. Sometimes this involves surgical removal of unsupported gingiva in order to make the pocket more shallow!
We’ve spent a long time looking at the precise nature of gingivitis and periodontitis. There’s nothing more critical in the fight against these diseases than to understand the root causes.
What other diseases are there that are perhaps less common that also affect the gingiva? One that we see occasionally that has a common name related very much to the analogies given above, is TRENCH MOUTH. It’s caused by the flourishing of a particular form of bacteria. It was most widely recognized during World War I in the trenches, where oral hygiene wasn’t one’s main concern. While in college I had a classmate that suffered from trench mouth, and for years afterward everyone called him “Trench”. He seemed to like the name, or at least never indicated otherwise, but he definitely didn’t like the condition.
The more official name of trench mouth is acute necrotizing ulcerative gingivitis, or ANUG for short. Acute means it comes on suddenly, you don’t get used to it. Necrotizing means something died, in this case some of your gingiva. And ulcerative means that oral ulcers are involved, which are basically like canker sores (visit chapter III.10). These descriptors make it sound like this condition probably looks really bad and feels worse, and that’s about right. The treatment is fairly simple, cleaning and antibiotic rinse.
Another situation that can happen is that the anaerobic bacteria in deep periodontal pockets get such a battle going with the immune system that there are lots of dead cells which form and must be released somehow. This exudate (pus again) will ooze out of the pocket when the gingiva are pushed in with the finger. They are is likely to be tender and will generally bother you enough to come into the dentist to see what is wrong. When these periodontal abscesses occur, it is a definite sign that more extensive periodontal treatment is really needed.
There are forms of periodontis that are found even in young people who have, for some reason, what is perhaps an increased sensitivity to particular bacteria. One bacterium which is often found associated with a disease called local juvenile periotontitis is called actinobacillis actinomycetemcomitans. It wouldn’t be worth spelling out except that the name is very cool. For some reason LJP, as it is affectionately called, seems to cause a particularly high rate of bone and attachment loss only for the first molars and lateral incisors. This is one of the mysteries of the human body, that there should be such site specificity. We don’t even know what kinds of cellular markers there could be that would differentiate the gingiva around one tooth from another, or maybe there is a simpler explanation? Hopefully the years and decades ahead will increase our understanding.
Now that we have looked in plenty of detail at the cause of various periodontal diseases we should look at how they are detected and diagnosed in the patient. We will only look at the most common, gingivitis and periodontitis. A familiarization with this material is critical if you are to understand what your dentist is telling you about your gum condition, and know for yourself the most appropriate treatment and home care.
The Monitoring of Gum Disease
More about periodontal measurements and diagnosis will be given in Chapter IV.4. For now, we’ll just take an introductory look at this issue.
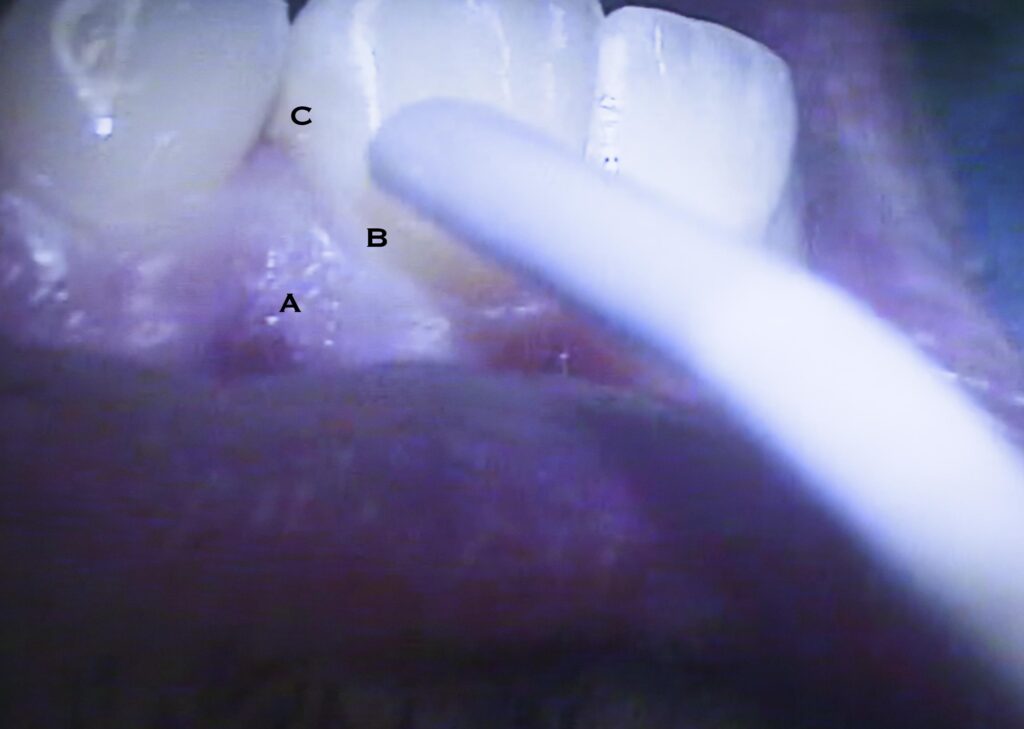
There are two tools that are used in the detection and diagnosis of gum disease, and periodontitis particularly. These are the periodontal probe and the X-ray film. The picture below shows a typical probe with painted bands 3 mm wide, being used to check the pocket depth of a molar. These are designed to allow measurement of the depth of the gingival sulcus or periodontal pocket. In the case of normal tissues the sulcus depth will be 1 to 2 mm. In the case of gingivitis, the swelling will often cause the sulcus to be deeper, but this is not due to the loss of attachment. In the case of periodontitis there are definite pockets which range from 3 to even 12 mm. Note that the only way you can have a 10 – 12 mm pocket is if the bone is lost from the tooth so far that the root apex is uncovered, and is in fact exposed to the oral environment through the pocket!
Generally, when using a probe to measure pocket depth, one records the depth from the gingival margin (the top of the free gingiva). You can place the probe in the pocket to the bottom and see where the margin of the gingiva rests against the side of the probe. That is the pocket depth and it is recorded at six places around the tooth – directly on the facial and lingual surfaces, and in the four corners.
You may have had the experience of pocket probing – and you may have felt a sharp pain when this was done. Sometimes it feels like the probe has a sharp point at the end and it is being pushed hard into the tissue – ouch! But, probes that are well made are quite rounded on the tip, and if the hygienist or dentist is careful, they are putting only the minimal pressure on the tissue at the bottom of the pocket. But – when the tissue is inflamed, like the splinter situation, just the smallest pressure can hurt. Your dental professional will know to be careful to avoid discomfort for you, but it may not be possible to avoid all pain because of your condition.
So, measuring the pocket depth is important, as it indicates how far down the bacteria can go, which determines the amount of air they are exposed to, and how pathogenic the bacteria are that can survive there. It is also a way to compare your gingival health from one visit to the next. If the pockets decrease, it probably means that the inflammation is decreased due to your more diligent home care, and removal of calculus at your last visit.
In the X-ray film below, most of the pictures demonstrate BONE LOSS, and you can also see CALCULUS on the root surface of many of the teeth. I’ve marked areas of calculus with a “T” and areas of bone loss with an “L”. This is a really severe periodontal case, and several teeth are about to be lost.

For moderate to severe periodontitis, dentists will use both X-rays and periodontal probing to keep track of the progress of the condition and effectiveness of treatment.
Diagnosis of Periodontal Disease
Attachment loss is also measured using the periodontal probe. When the tooth newly erupts in youth the periodontal tissues are attached to the tooth on the enamel surface. Over the years this attachment area migrates farther down the tooth toward the root. The dividing line between the crown of the tooth and the root is where the enamel and cementum covering of the root meet – called the cementoenamel junction, or CEJ. If the attached tissues have migrated onto the root, the CEJ is exposed in the pocket and we are said to have attachment loss. The distance in mm from the bottom of the pocket to the CEJ is the amount of attachment loss.
With simple gingivitis, there is NO attachment loss, by definition – there is inflammation, swelling and bleeding – signs of infection only. With periodontitis there is infection with the signs above, WITH attachment loss. The severity of the periodontitis is rated based on the amount of attachment loss accompanying the inflammation. You have moderate periodontitis if your attachment loss is in the 4 – 6 mm range, and severe above that.
Recall that IF you have deep pockets and loss of attachment, you do not necessarily have periodontitis. If you have NO signs of inflammation, you do not have active, current disease, only a history of the disease, which cannot be erased.
There are other clinical observables which are also expected for periodontitis, and are used to confirm the diagnosis and classification. One is BONE LOSS, as we’ve discussed. The extent to which the bone has migrated down the root will reflect the pocket depth generally, and attachment loss specifically. Sometimes there is a defect in the bone level, a particular place where the bone loss is greater in some areas of the mouth than others, but the generalized bone loss should correspond to the periodontal class,, slight, moderate and severe.
Also, since the boney support is being lost, the teeth will probably become mobile as well. The evaluation of MOBILITY is important in the classification and diagnosis of periodontitis. And, the other observation we make is the degree of FURCATION INVOLVEMENT. Recall that the furcation is the place where the roots of a single tooth join at the top. If the bone and gingiva have receded, then the furcation can become uncovered. These sites are difficult to keep clean and are areas where recurrent infection leading to decay and further periodontal attachment loss is likely to occur.
The risk of tooth loss is so much higher for teeth where furcations are involved, that we will spend some time in the next section paying more attention to these concerns.
Sites of Periodontal Infection
All major studies in the field of periodontal health that investigate the relationship between professional treatment and/or home care and longevity of the teeth note that the teeth must be divided into two groups. This grouping is based on whether there is a furcation. For example, all molars and the upper first premolars (bicuspids) have furcations. The other premolars and all anterior teeth have only one root, typically, and thus have no furcations. The former of these groups always demonstrates loss of teeth at a higher rate.
It is likely that this more rapid tooth loss for the teeth with furcations is due to several factors, most of which have to do with the fact that exposed furcation areas are hard or impossible to keep clean. One major problem is that decay in the furcation areas almost certainly results in tooth loss due to the unrestorable nature of the area. Another problem is that calculus removal in these areas is much more difficult than on other root surfaces, therefore any periodontal disease problem will certainly be exacerbated here. Also, it must be considered that teeth with furcations generally have one or two roots that are shorter than the anterior roots, therefore any bone loss can more quickly uncover these roots. When the apex of the root is exposed to the periodontal pocket, infection is often transferred from the pocket into the canal system of the tooth. This may also initiate the decision to extract.
Certainly it is commonly seen that patients have lost many molars and premolars but still have all of their anterior teeth. Often this is due to occlusal decay from their earliest days, but also it is consistent with the pattern of loss due to periodontal disease. Of the remaining anterior teeth, most often the lower incisors are quite mobile. The tiny, thin roots of lower incisors just won’t keep them solid when the bone support drops below the half-way point on the root (the X-ray above illustrates this point). Again, clinical observation suggests that most bridges and partial dentures that replace the lower incisors are necessary due to the ravages of periodontal disease. On the other hand, most bridges and partials that replace the upper incisors are made to make up for the ravages of bicycle accidents, ice hockey, or barroom or household confrontations!
Treatment Options
We will quickly look here at various treatments designed to correct periodontal problems. More detail on periodontal therapy will be covered in Chapter V.12, but we shall introduce the subject here.
Antiobiotic therapy – the simplest possible treatment for periodontal disease. Unfortunately, just taking some pills won’t affect the slow, steady damage due to bacterial colonization in periodontal pockets. Even if you can stop the growth of these bacteria for a time, soon they will be back at work. The use of antibiotics to flush out pockets where there is evidence of abscess is more firmly established. Many practitioners will irrigate these deep pockets with solutions of tetracycline. But, if the presence of antibiotic is helpful in these situations, it is only to correct an acute problem – it will have no effect on the underlying disease process.
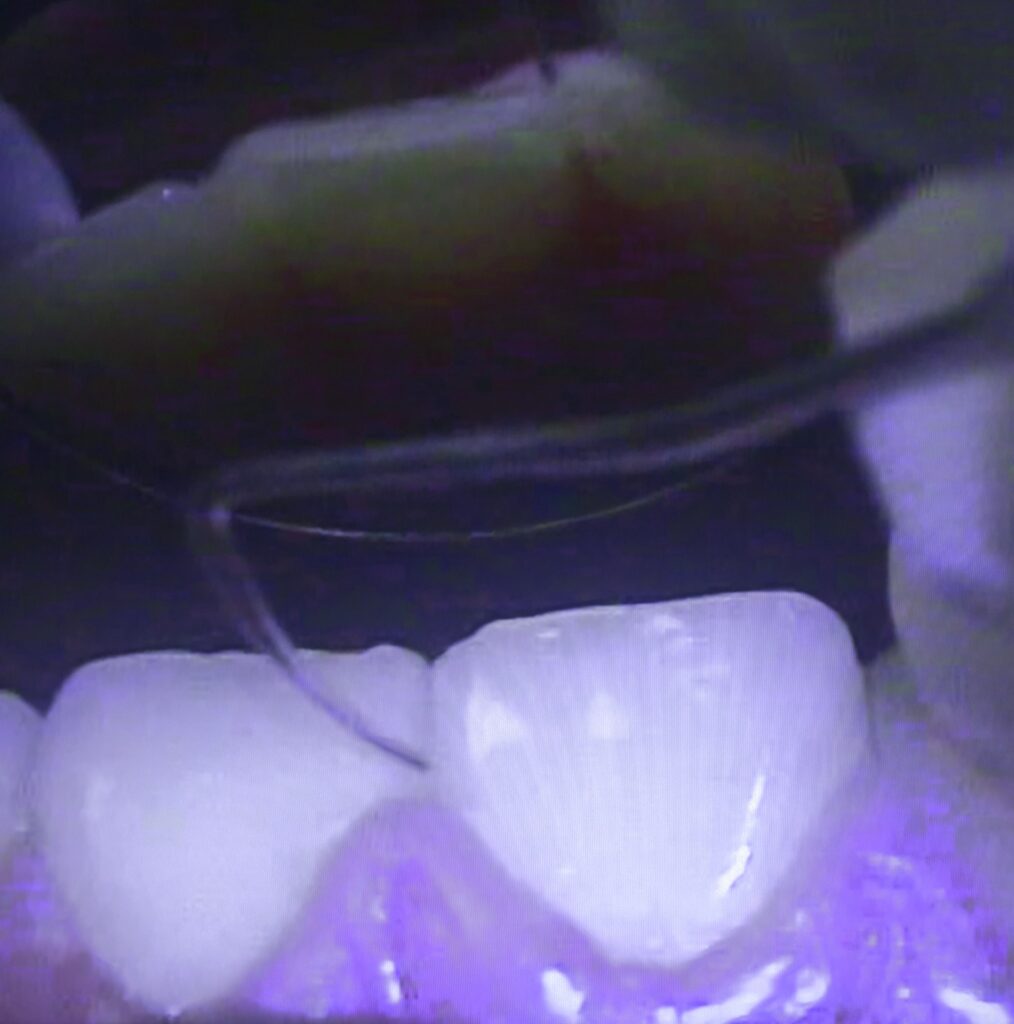
Root Planing – the most common periodontal therapy. This procedure is normally done with hand instruments designed to reach down into the pocket and then scrape the root smooth as the instrument is dragged back up the root surface. The illustration below shows a cross section of the functional part of the instrument as it is properly rotated against the root during a planing stroke. Note than an error in rotation can cause the instrument to miss the calculus and instead tear the tissue of the pocket. Root planing is a procedure that requires great skill, but it is also quite effective.
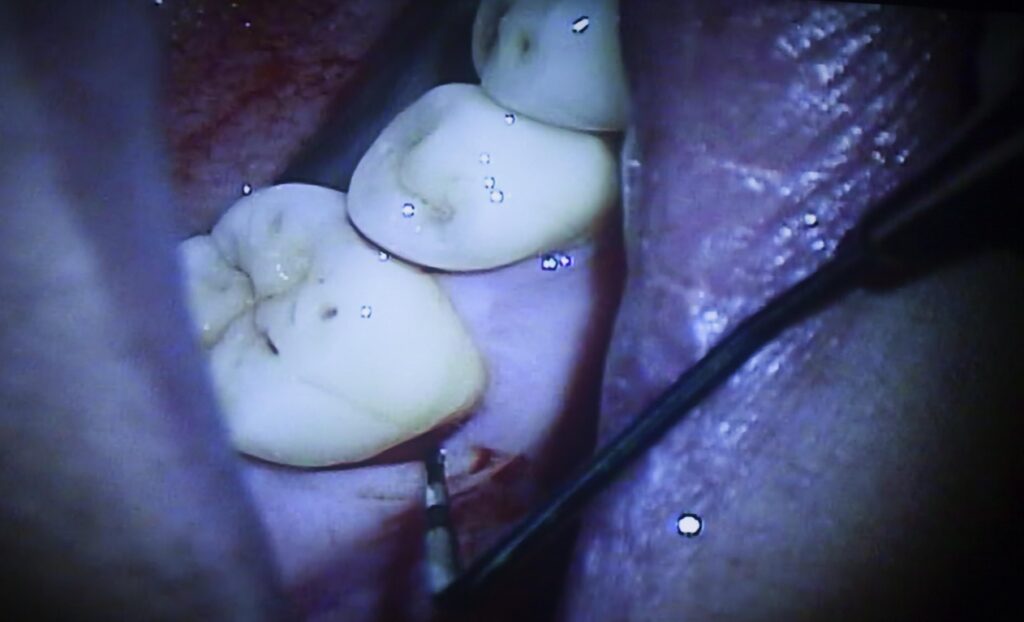
Surgical cleaning – when root planing is not complete enough through the pocket. Generally, when the pockets are deeper than 6 mm even a highly skilled professional cannot clean the root surfaces to the depth of the pocket using just a curette. Thus, traditional root planing through the pocket may not arrest the periodontal disease in these areas. When initial root planing treatment is found not to reduce pocket depths in some areas, a surgical approach is the only possibility. Here the gingiva are cut away from the teeth and bone and are folded back to expose the root surfaces to direct approach. Now the roots can be planed thoroughly to the bone level without question as to the resultant smoothness in all areas. The tissue must be sutured back into place afterward, and there is significant post-operative discomfort often experienced, and a longer healing process. I never liked to refer my patients for this surgical procedure because of the discomfort afterward – so best to avoid!
Bone implants – when a boney defect cannot be expected to fill in by itself. While root planing can arrest the progress of periodontal disease, it will not result in the return of attachment or bone loss that has already taken place. But, sometimes, it is possible to surgically implant bone material (either harvested from the same individual – generally from the hip – or from someone else). In the case of a graft from another donor, the bone is sterilized and often freeze-dried. Sometimes defects in the bone can be filled in successfully using these implant powder products. Interestingly, if successful, the implanted bone is usually replaced by naturally bone eventually by the natural remodeling processes in the body. Unfortunately, the predictability of bone implantation is often not good, but the technique works well in many instances.
Guided tissue regeneration – where artificial membranes are surgically placed to force new attachment. Often postsurgical attachment is via cells that are on the surface of the gingival tissues, and not a result of fibrous connection of the tooth to tissues deep within the gingiva. In order to form “a more perfect union” sometimes some membraneous material, like Goretex (yes, the same stuff used in up-scale rain jackets and sneakers) is tied against the tooth as a collar during healing from surgical root planing. This may keep the cellular part of the gingiva from reforming down the root surface, while allowing attachment to be made from the deeper tissues. A difficult concept, and not always successful, but generally worth a try when done by the right person, and in carefully selected circumstances.
Extraction – what the periodontist REALLY hates to do, but it is the ultimate solution to periodontal disease. The person whose job it is to save teeth from periodontal disease doesn’t like to admit failure any more than do the rest of us. He/she will fight “tooth and nail” to keep from giving up on a tooth. But sometimes there just isn’t anything that can be done, especially if the bone loss is so severe that the tooth just has no support. You can picture the surgical situation where the gum tissue has been folded back and the only thing holding the tooth in the body is a tiny bundle of nerves and blood vessels. The periodontal specialist will generally have all necessary extractions done before proceeding with therapy on the remaining teeth.
I once saw a patient where the only thing keeping one tooth in the mouth at all was the fact that it was attached to another tooth by a bridge. In fact, I could run a string of floss completely UNDER the tooth from side to side – so not even nerves or vessels were connected anymore!
Prevention – Home Care
This is where you come in. Proper care of the teeth is taught to older individuals largely in the defense against gum disease. Chapter V.12 will cover this area in more depth, but it is important to note here that the arrest of damage caused by periodontal infections is your responsibility. We often tell patients, even after aggressive periodontal surgery, that the treatment we give will have no lasting effect unless THEY take over from there. The plaque layer must be removed from all tooth surfaces once every day, or calculus formation will start over. The dental professional can attempt to make the pockets shallow enough to permit you to keep them clean, but you must do so!
Concluding remarks
There is sometimes a fine line between overtreatment and undertreatment of periodontal disease. But, generally, when you have several pockets that are approaching 6 mm, and there is any evidence of subgingival calculus (in the pocket), then root planing is in order. More and more general practitioners are starting to realize that this is part of an appropriate comprehensive treatment package and will make sure that the therapy is done, either by themselves, a licensed dental hygienist in their employ, or by referral to a periodontist. Most dentists can also recognize when the periodontal situation is one that is not likely to be solved by initial root planing therapy. In these cases it requires a detailed discussion with the patient to evaluate their determination to save teeth. If there are some teeth that might be saved by aggressive therapy by a periodontist, and the patient REALLY doesn’t want to lose them, then referral is appropriate. But if the patient is quite willing to lose the teeth, then the added cost and discomfort of sophisticated periodontal therapy is not recommended. More and more dentists are learning to evaluate the potential for saving teeth and performing procedures and referrals as needed.
On the other hand, there have been practice management groups that are hired by dentists to help increase office productivity, that actually teach OVERdiagnosis of periodontal disease. In cases where the dentist is not as familiar with the fundamental basis and appropriate therapy of periodontal disease, they can be mislead by these groups. There have been many cases where patients are treated by expensive root planing therapy when it is not needed and certainly not effective. In fact, if there are some areas that probe relatively deep (say 4-5 mm) due only to gingival swelling of gingivitis, but where the bottom of the sulcus is still on the enamel, root planing, as such, cannot be done! You simply can’t plane a root when it is not accessible. Any procedure done in this case must be referred to as scaling or deep scaling, in that there is no treatment of the root itself, and you must be charged as such!
It is hoped, then, that this complex chapter will help you with the understanding of your periodontal condition (and you are likely to have one) and its appropriate treatment. Just remember that gum disease is caused by bacterial infection, and these bacteria are VERY difficult to eliminate or control. Effective treatment requires a high level of knowledge and skill on your part, and determination, and also on the part of your general dentist. Learning from this website will provide you with the requisite knowledge. Your dentist or hygienist can teach you the skills. If you then PARTICIPATE in the professional phase of your treatment and find the motivation to perform the appropriate home-care, you will do doubt be successful in the arresting of the periodontal disease process.
Remember, the difficult thing about periodontal disease is that you can’t expect the dentist or periodontist to eliminate it for you. You must be involved in the cure or it will recur and eventually result in the loss of teeth and the creation of oral complexities that are much more challenging to correct.