You may want to supplement whatever you find in this site for Supporting Structures for the Teeth with a section on teeth in Wikipedia – they cover many important topics with good references to the literature in areas you may want to delve into more deeply.
Organization of this Chapter
You may Skip to Whatever Subject Interests You Now
Basics
The Gum (Periodontal) Tissue
Periodontal Ligaments
Bone – The Alveolar Ridge
Bone – The Mandible
Bottom Line for Supporting Structures
………………………………………………………………………………………………………………………….
The Basics
While the teeth are the primary interest of our study here, the supporting structures for the teeth – that hold them in the mouth – are obviously vital to the retention of the teeth. If we develop diseases of the bone or gum tissue, the teeth may be lost.
Here we will simply review the design of the tissues that help hold the teeth in place, and then in the next Section we will look in great detail at various disease states that impact the health and function of these tissues.
In Chapters III.2, IV.4 and V.12 will be given more structured accounts of the diseases, the diagnosis and the treatment of gum disease.
In Chapter III.10 will be considered diseases affecting the bone.
The Gum (Periodontal) Tissue
There are two kinds of “gum tissue” in the mouth, the mucosa and gingiva. The mucosa covers the inside of the cheeks and the bone, but is not attached to it. The gingiva is attaches to the bone and to the teeth. Inflammation of the gingiva is called gingivitis, a term familiar to all of us, thanks to television advertising.
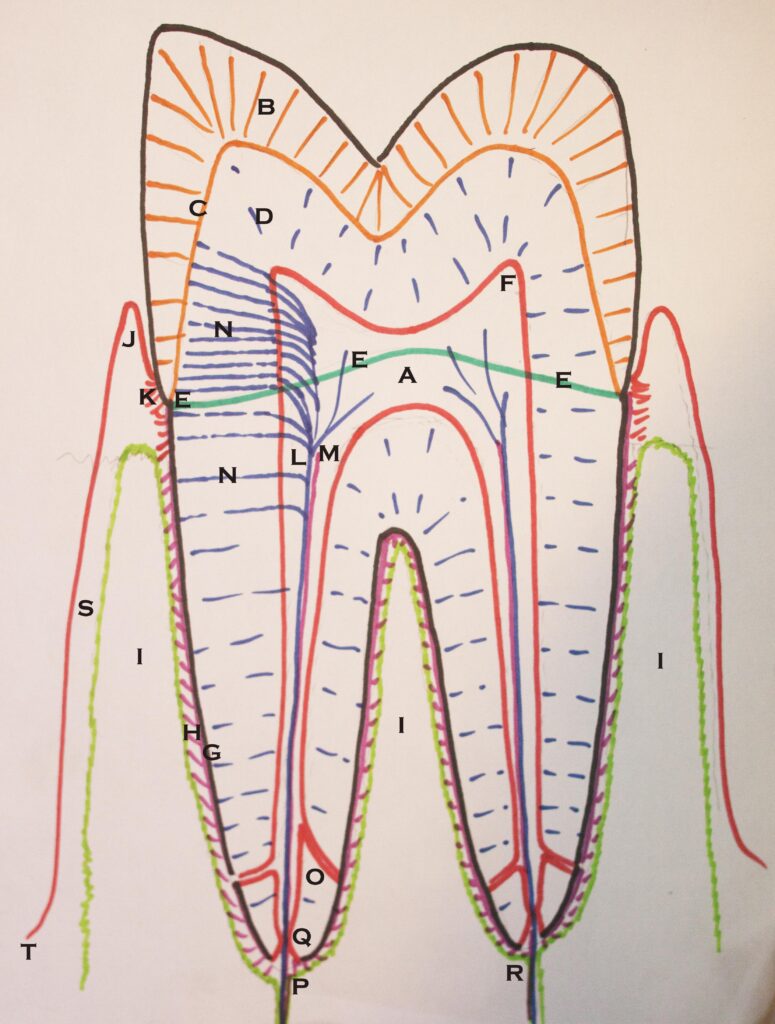
Our main concern is the gingiva. Since the teeth are anchored in bone, and the gingiva attaches to both bone and teeth, it provides a seal around each tooth as well as being a Supporting structures for the teeth. The diagram below shows how the gingival tissue attaches to bone and tooth. Note particularly there are cells that cover the internal surface of the gingiva. These cells provide protection for the fibrous structures of the gingiva from the bacteria of the mouth. Also, these cells form an attachment to the tooth itself. In a healthy mouth the surface cells of the gingiva rise to a sharp peak called the free gingiva, and then descent down the side of the tooth to attach to the enamel. Fibers from the gingiva attach to the root surface of the tooth between the enamel and the bone level about 2 mm lower.
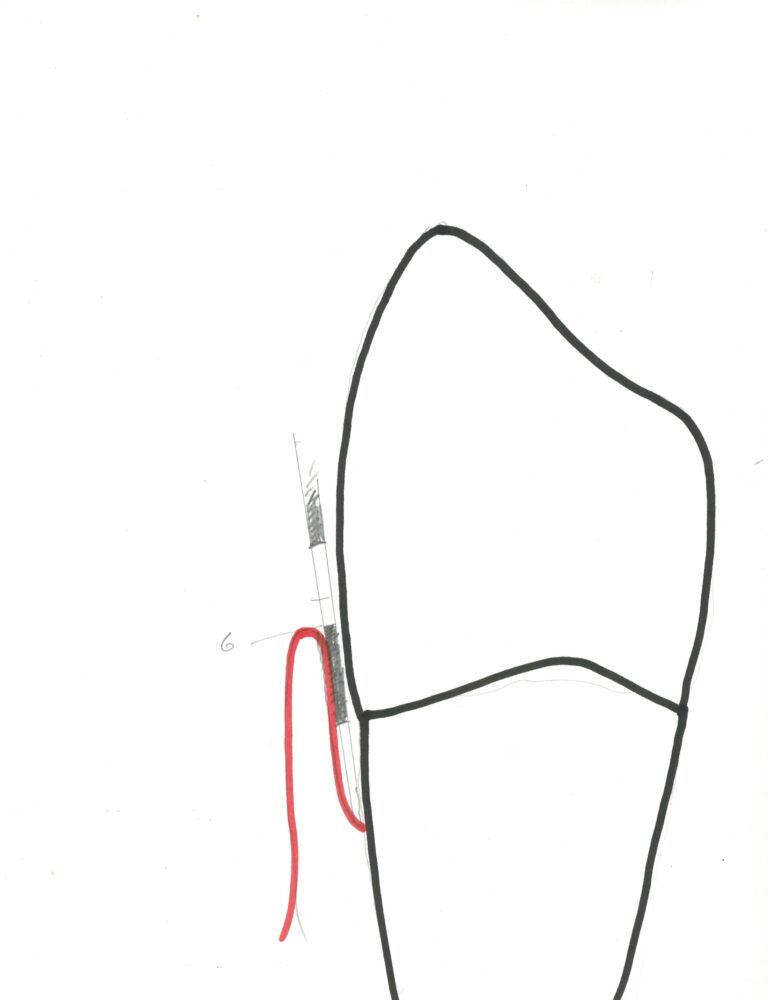
The attachment of the gingiva to the tooth keeps bacteria from penetrating to the bone, but it is still possible that bacteria will colonize in the pockets bounded by the free gingiva. However, when the pockets are small, 2-3 mm, the bacteria that tend to grow do not cause serious, or irreversible damage, only the inflammation we call gingivitis. On the other hand, in cases of more serious gum disease, called periodontitis, the pockets become deeper and are capable of supporting the growth of bacteria that must live out of contact with air. These anaerobic bacteria can be quite damaging.
The drawing below shows what the pocket inside the free gingiva looks like with moderate periodontal disease. Note the greatly deeper Comparing the drawing here with that for the healthy case on the previous page makes it clear that cleaning of the pockets cannot really be adequately done when the pockets are deep. Frequent professional care is necessary in these cases, and the goal of treatment is the reduction of the depth of the pockets. The loss of attachment, however, is not considered reversible.
Periodontal Ligaments
The tooth root is also attached directly to the bone by microscopic fibers called ligaments, label “H” on the diagram at the top. There is a small space between the roots and the supporting bone, and the ligaments support the tooth like a cushioning net. It is THE primary supporting structure for the teeth.
Due to the slight “give” in the ligaments, they act like shock absorbers. In this way biting a hard object does not “jar” the jaw bone, but impacts are deadened. Later we’ll talk about implants, and this is the biggest difference between a natural tooth and an implant – the existence of cushioning ligaments.
More detail on the periodontal ligaments is found in Chapter II.2.
Bone – The Alveolar Ridge
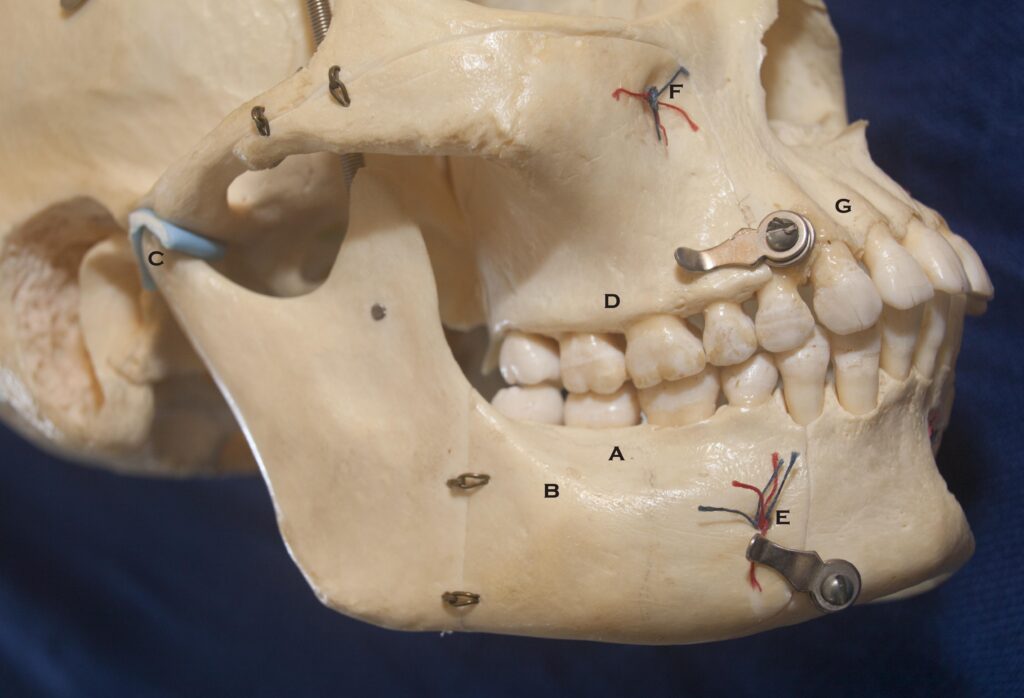
- A – The Alveolar ridge of bone on the mandible which holds the roots
- B – The Basal bone of the mandible
- C – The Condyle of the Temporomandibular Joint, with simulated disc
- D – Alveolar ridge of the maxilla – the “upper jaw”
- E – The exit of the mental nerve through the mental fossa
- F – The exit of the infraorbital nerve through the infraorbital fossa
- G – Note the thin layer of bone over the roots of the upper front teeth!
The arch-shaped rows of upper and lower teeth are supported in bone. The bone that is immediately surrounding the roots is called the alveolar ridge. This ridge forms the upper border of the jaw bone, and the lower border of the bone surrounding the sinuses and nasal cavities. It is important to realize that this alveolar bone is present only to support the teeth. When the teeth are gone, the bone will resorb and virtually disappear. That is one of the biggest challenges to wearing complete dentures when you have lost all of your teeth. The ridge will eventually go away and the dentures will have to be relined frequently to fit the new shape of the ridges, and as the ridges flatten the denture becomes more and more unstable – and they may need to be stabilized later by placement of implants in the remaining bone.
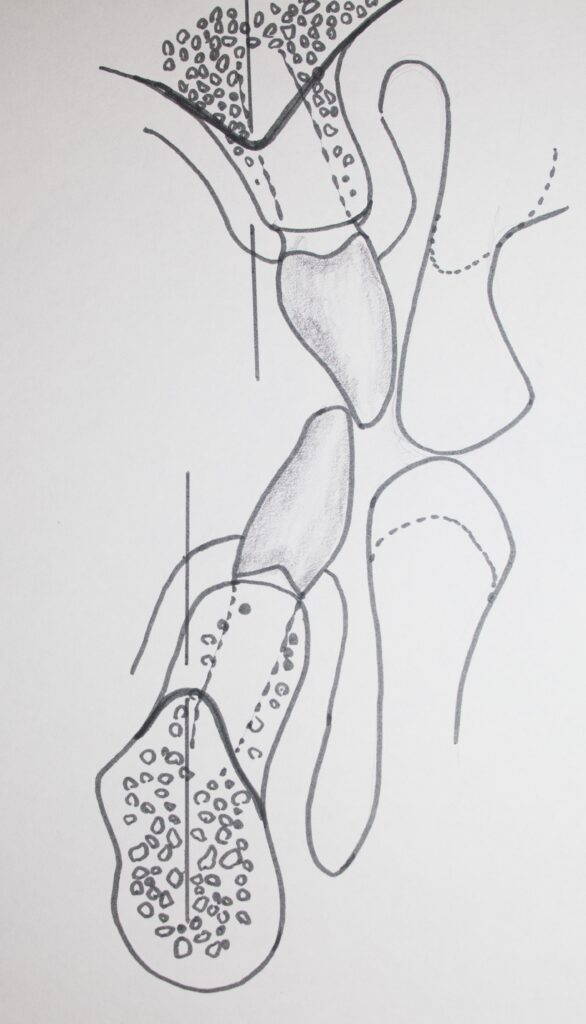
When the bony ridge recedes due to gum disease, then areas of the root may be uncovered. Of particular risk is the exposure of the furcation areas between roots of, particularly, the molars. We have seen already that these areas are particularly prone to decay.
Another concern regarding the level of bone on the tooth is the space between the bone and the bottom of the pocket. Whatever the level of bone, this distance is generally around 2 mm. When decay goes into the pocket near the bottom and a filling has to be placed closer than 2 mm to the bone, then the tissues will react adversely, leading to chronic inflammation and discomfort until the situation is corrected, generally by removing some bone. The importance of this principle has resulted in the 2 mm space given a special name, the BIOLOGIC WIDTH. In the top diagram it is the space between the letter “K” and the top of the bone, colored in green.
Bone – the Mandible
Having discussed the alveolar bone, that which actually holds the teeth in place, let’s look at the mandible, the jaw bone. The picture above shows the shape of the mandible. The alveolar ridge can be seen on the upper edge with the teeth inserted. The pointed area, called the coronoid process, is where one of the major closing muscles is attached. The muscle actually pulls this area of bone away from the body of the mandible – forming the protrusion to which is it attached. When you get a headache in the area of your temples, it may be caused by stress and jaw clenching of this muscle, called the temporalis which makes the muscle sore.
The roughly ball-shaped part of the mandible, called the condyle “C” above, is what inserts into the socket of the joint near your ears. Feel the area in front of your ear while opening and closing your mouth. You can actually feel the condyle moving in its socket!
While there are three powerful muscles that cause the mouth to close, one connected to the coronoid process and two pulling up on the mandibular angle (one inside the jaw and one outside), there are weaker muscles connected to the chin which are responsible for opening. Can you think of another reason for forceful opening of the mouth other than to separate the teeth from a tightly adherent piece of caramel?
There are also muscles attached to the necks of the condyles that cause the jaw to shift from side to side, or to move forward. They are directly controlled by the brain to make sure that the teeth are positioned correctly relative to each other as the mouth closes and the teeth tough, as in swallowing.
We’ll discuss this more in Chapter II.4 and Chapter II.5 to follow.
The picture below shows more detail about exactly HOW the teeth are anchored into the mandible. You can see the roots in the bone, and a denser layer of bone around each root, which is all part of the alveolar ridge. You CANNOT see any space for the periodontal ligaments that support the tooth in the boney socket, but the space is there. It just doesn’t take much space for these very short fibers.
Most of the bone seems very porous, other than the surfaces, which are more dense cortical bone.

Bottom Line for Supporting Structures
It should be clear that the design of the tissues that support the teeth in the arch is very complex. It needs to be.
The tooth can well be considered part of the bone – it is connected to the bone in the upper and lower jaws in much the same way that the bones of the skull are connected together, with fibrous tissue. The difference is that the teeth actually PENETRATE the covering soft tissue layers and are exposed into the oral environment.
If you had a compound fracture of your leg, and the bone were sticking out through the skin, it would be similar – except the skin is much cleaner than the mouth.