I was looking for a good external reference so you could link for more exploration of the topic of Periodontal Charting – but this seems to be the most useful at this point.
Organization of Chapter
Basics
Pocket Depths
Attachment Loss
Inflammation
Diagnosis of Periodontal Disease
Mobility
Bone Loss
Recession
Furcation Involvement
The Bottom Line
………………………………………………………………………………………………………………………
Basics
To track the progress of periodontal disease in a patient, the dentist will make a variety of measurements. There is a need to assess the support of the tooth in the bone, and the connection of the gums to the tooth. As periodontal disease progresses, these measurements will change and appropriate measures may be taken to stop this – through professional therapies and home care.
Each of the measurements that are needed for a complete charting of a patients condition will be described below.
Once you get into an age range where periodontal disease is typical, or you have any early-onset disease, your dentist will keep a detailed record of your condition.
Explore the chapter on Periodontal Disease for more information on the CAUSE of problems, and the chapter on Periodontal Therapy for understanding about what we do about it.
Pocket Depths:
Refer to the diagram shown below.
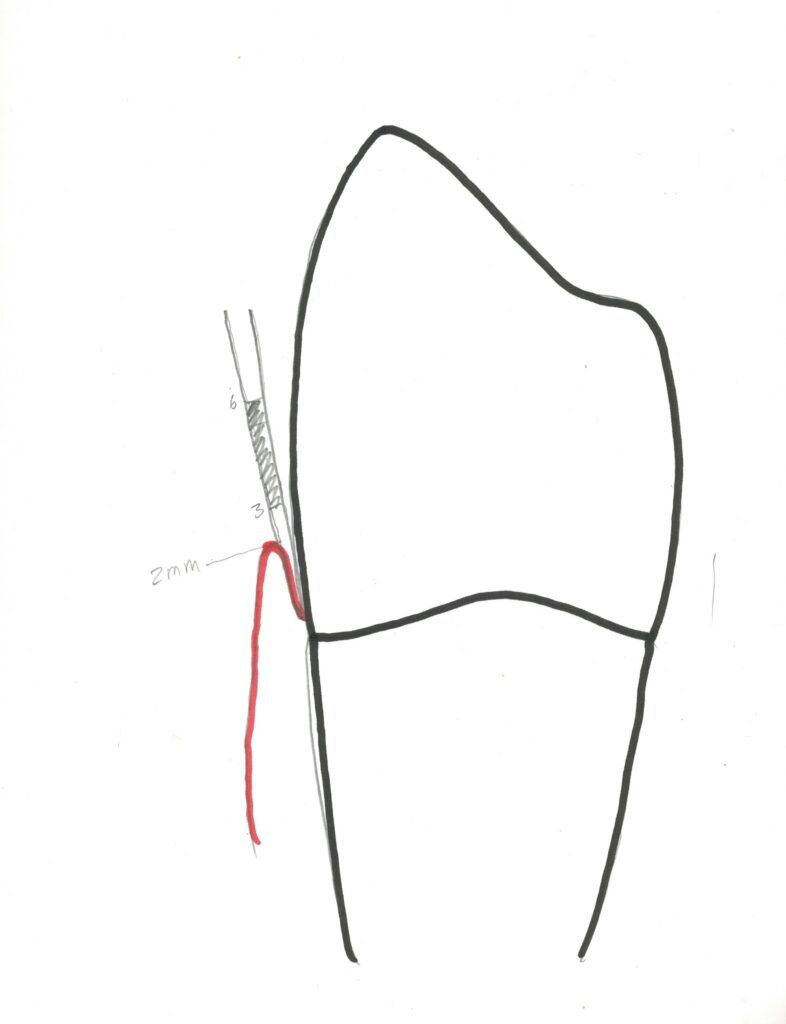
For this the dentist uses a periodontal probe, which is marked with millimeter lines in a variety of patterns. The dentist inserts the periodontal probe into the space between the gingiva and the tooth and GENTLY moves the probe until it rests on the bottom of the pocket. If you have a lot of calculus buildup, then it may not be possible to get the probe to where the soft gingival tissue connects to the tooth, or it may make it more difficult.
It would be best to remove the calculus deposits from the pockets before measuring depths, but if you are a new patient, this initial reading before any suggested therapy is of value in the diagnostic process. If you are a continuing patient of record, it is typical that if a hygienist does a routine cleaning (which does not reach down much into the pocket), she will check your pockets after this is done.
We discussed subgingival calculus in Chapter III.2.
When your pocket depths are being measured it may be quite painful – but this can be minimized. If you have lots of calculus deposits, that means that there is a lot of bacterial presence in your pockets – and that means there will be an inflammatory response by your body. This response is like your body is responding to a splinter – swelling, redness, tenderness. You may feel that the periodontal probe has a really sharp end, when it is generally designed to have a very rounded end to create as little discomfort as possible. Also, it may feel that the dentist or hygienist is pushing hard down on the probe, which they should not be. They MIGHT be doing this, but it most likely feels that they are when they are really being quite careful. When you jump they will certainly notice and attempt to minimize your discomfort. Nonetheless, if your gums are badly swollen and bleeding and painful, they still need to establish a baseline reading that can be compared with subsequent readings as work is done to correct your condition.
Now – a typical pocket depth for a patient that has had no periodontal disease and does not have inflamed gingiva (gingivitis) will be around 2-3 mm. Refer to the diagram above – this is the distance measured between the highest point of the gingiva (the free gingival margin), and the bottom of the pocket. It can be read directly from the side of the probe.
This measurement is made SIX times around each tooth for the standard charting. On the facial side of each tooth, it is measured close to the adjacent tooth on each side, and once in the middle. This is also done on the lingual surface. For the measurements near the adjacent teeth it is a little tricky, because the tip of the probe must be positioned as much as possible directly underneath the contact between adjacent teeth, while the probe higher up leans against both of the adjacent teeth in what we call the embrasure.
When these six pocket depths are charted, a periodontal chart has a diagram showing the teeth and boxes for each set of measurements, facial and lingual, on every tooth.
Since the pocket depth is measured to the highest point of the gingiva in each site, if the gingiva are swollen, it will increase the reading. It is the DECREASE of the pocket depth by reducing the swelling that we look for as progress. Note that the decrease only reflects the decrease in swelling – it does NOT reflect any change in the location of the connection of the gums to the tooth at the bottom of the pocket, because this does NOT CHANGE SO TO LOWER THE READING.
We do not expect that the ATTACHMENT of the gums to the tooth will ever improve no matter how well you care for your gums. If the attachment has migrated toward the root or onto the root due to chronic periodontal disease, it is not going to move back up! The best you can do with great home care and regular professional therapy is to keep the attachment from being lost even more than it has been.
When a dentist looks at your periodontal chart, he/she will be looking to see how deep the pockets are. Deeper pockets may indicate you have really swollen gums, or that you have attachment loss where there is movement of the bottom of the pocket, or both. One of the consequences of having a deeper pocket, is that when there is calculus in the pocket, it is more difficult to remove. This was discussed in Chapter III.2 and will be in detail in Chapter V.12 where periodontal therapy is presented.
As was indicated, a pocket depth of 2-3 mm is considered normal and healthy. Anything approaching 6 mm is indicative that you have progressing periodontal disease, and it will make it more difficult for the dentist or hygienist to remove any calculus in that pocket, when deeper subgingivally. When more than 6 mm, say 8 or 10 mm, it indicates a more severe problem that may take a periodontist to address.
Again, the goal is to receive therapy and do home care to the extent that the progress of the periodontal disease will be HALTED!
Measuring Attachment Loss:
When your tooth first erupts, the attachment between the gums and the tooth at the bottom of the pocket is on the enamel surface. As it migrates apically (down the tooth toward the root), it will eventually be AT the CEJ (the junction between the enamel and the cementum covering of the root). You are NOT considered to have “attachment loss” at this point.
As soon as the attachment migrates onto the root, and a space can be detected between the CEJ and the bottom of the pocket, THEN you are said to have attachment loss.


For the dentist to MEASURE the attachment loss requires some tactile skill. The probe is inserted into the pocket and the dentist FEELS for the change from the enamel (curved and smooth) to the root (straight and textured). When the dentist detects this CEJ, he/she then looks to see how much FARTHER the probe advances from that point to the pocket bottom. This is the number that is recorded on the chart, and is the attachment loss, by definition.
Basically, if the dentist can FEEL the root surface below the CEJ with the probe, you have attachment loss.
When there is significant calculus deposited at and around the CEJ, it makes accurate determination of attachment loss more challenging, but your dentist should be able to get a pretty good idea.
Recording Inflammation:
For each pocket depth measurement on the chart, the dentist or hygienist will place a little red dot on the number if there was any bleeding when the probe was placed in the pocket. One of the important signs of inflammation is the tendency to bleed upon probing.

Other signs of gingival inflammation are color changes, swelling, loss of the “stippling” which is the kind of uneven reflective appearance shown on the picture above, and loss of sharp edges of the gingiva against the tooth.
Diagnosis of Periodontal Disease:
The diagnosis for each tooth is also included on the chart and these diagnoses range from gingivitis to mild, moderate, or severe periodontal disease.
The diagnoses are made strictly according to the numbers on the chart. If any location on a tooth has inflammation recorded along with attachment loss, then the tooth is considered to have active, current periodontal disease. The precise definitions vary from agency to agency, but, typically, if the attachment loss is 1 or 2 mm, with inflammation, then you have mild periodontitis on that tooth. If the attachment loss is 3, 4 or 5 mm, that indicates moderate periodontitis. If you have 6 mm or more attachment loss with inflammation, that shows severe periodontal disease.
There are other indicators that are charted as well, that will likely be found to be consistent with the diagnosis, based solely on attachment loss and inflammation.
Tooth Mobility:
The teeth, as supported by the bone, are designed to remain pretty much in place with application of lateral forces. If I were to push on a lower first molar from the facial and lingual sides alternating, the tooth MAY rock back and forth. If it rocks significantly, it may be an indication that the bone support has been lost for the tooth, due primarily to periodontal disease.
A movement that is just detectable is considered Mobility Class I. Now, this depends to a great extent to how well the dentist applies the forces, and how fine he can detect movement with the visual acuity of his vision – but if a dentist can detect a back-and-forth movement even of .5 mm, that is considered class I, or mild mobility. YOU have at least class I mobility right now.
The measurement is the total distance moved from one extreme to the other.
If I were to push on your tooth back and forth and it moved 1-2 mm, that is considered moderate mobility, class II. And if it were to be 3 mm or more, it would also likely display DEPRESSABILITY, where the tooth can actually be pushed farther DOWN into the bone, indicating that it is not RESTING on bone at the apex. This is a severe mobility and indicates considerable bone loss.
Bone Loss Measurement:
The bone loss can be measured directly from radiographs. The bone level is ideally and originally 1-2 mm from the CEJ, the junction between the enamel and root cementum, easily seen on the X-ray. From the the CEJ to the apex the root is divided into three sections. If bone level is within the top section, it is considered mild bone loss, whereas if it is observed in the middle or apical thirds, that is moderate or severe bone loss.
Recession:
While the attachment, or bottom of the pocket, is on the enamel initially and migrates apically with advancing periodontal disease – the gingival free margin is higher than that on the side of the tooth, but also migrates apically with advancing disease. Once the gingival free margin has receded beyond the CEJ and the root of the tooth can be seen, that is considered recession. The millimeters of recession is also indicated on a complete periodontal charting.
Recession is that phenomenon which allows the black triangles to show underneath the contacts between adjacent teeth – and this can have an important esthetic impact for the anterior teeth. But, for any tooth, the more recession you have, the more the roots of the teeth are visible, and this doesn’t look too good either.
Also, many people are familiar with the consequences of recession because their teeth become SENSITIVE! This sensitivity shows up as a sudden pain when you drink something cold, or even inhale cold air.
The Sensitivity can be controlled by a treatment at the dental office, where a kind of varnish is painted on these areas, but it also helps to use a toothpaste that is designed to minimize the discomfort. The best known such toothpaste is Sensodyne. The idea is that these pastes have something in them that will fill in the porosity of the surface of the root, and may keep the nerves in the dentin of the root somewhat isolated from their environment.
Furcation involvement:
This is the last measurement that we will note here. As the gingival attachment migrates apically, for teeth with multiple roots (molars and upper first premolars, typically), the place where the roots join, near the CEJ, may become exposed to the oral environment. You don’t need to have recession for this to happen, but the bottom of the pocket being in the area of the furcation will make these areas exposed.
Exposure of furcations does two things, and both are bad. First, it allows plaque to be deposited in places where it is difficult to remove, because it is difficult to brush here. Second, there is a significant chance of decay starting in these areas, and they are very difficult or even impossible to restore – leading to the loss of the tooth.
I’ve had patients whose attachment on the posterior teeth is so severe that a small brush, like a tiny baby bottle brush, can be inserted through the furcation from one side of the tooth to the other. And, if there is this much furcation involvement, it is important to keep the area scrupulously clean with these little brushes, because if you don’t, decay and advancing periodontal disease can certainly cause tooth loss.
The Bottom Line
Not everyone needs the complete charting procedure outlined above. Certainly, if you have a tendency toward periodontal disease, and your dentist measures some 4, 5 and maybe 6 mm pockets with definite subgingival calculus and some attachment loss, then you should have complete charting done so that your progress can be monitored over the years. Without this monitoring, it is likely that you will not be as diligent in your home care, and even possible that your dentist will not pay as much attention as he/she should, and you will progress more rapidly toward tooth loss.
One final note – if you have deep pockets and significant attachment loss and NO inflammation, you do NOT have periodontal disease. You certainly have a HISTORY of having had periodontal disease, but it is not currently active. This is certainly indicative that you are taking good care of your teeth at home, and likely getting timely cleanings as necessary at the dentist’s office. You will not get your attachment back. Your recession will never look better. But, your condition and appearance will not look worse!