Wikipedia has an excellent section on Dental Extractions, along with a listing of complications and ample references to the primary literature.
From a personal standpoint I am thinking now about getting a tooth extracted. My lower left wisdom tooth, #17, has separated from the adjacent tooth and food gets packed in there every time I eat. The tooth is not useful in chewing, as #16 (the opposing tooth) is gone, and the area aches a lot and requires constant attention. As it is fully erupted and the roots are not bulbous it should be an easy job – but I resist going to the dentist to get it done – especially now. I DO know a dentist who I feel takes fully acceptable precautions in the office for the Covid Pandemic – but still I hesitate ….
Organization of this Chapter
You May Skip to Whatever Subject Interests You Now
Why Get a Tooth Extracted? 11 Reasons
Factors Determining the Difficulty of an Extraction
Basic Method
Challenging Situations – 6 of them
Methods of Extraction
Recovery from an Extraction
Routine
Bleeding
Suturing
Bone Grafting Situations
Bottom Line for Dental Extractions
………………………………………………………………………………………………………………………
Dental extractions can be practically unnoticeable or quite traumatic, but some teeth get to the point where they just are no longer needed, and would compromise your comfort and health to keep them in. As such the COST of extractions can run from the cost of a take-out dinner to something far surpassing the best restaurant meal you’ve ever experienced.
WHY get a Tooth Extracted?
Only Roots Left
Tooth Riddled with Decay
Decay in the Furcation between the Roots
Periodontal Reasons
Vertical Fracture into the Root
Tooth is not Needed
Keeping the Tooth would be too Expensive
Tooth is Impacted
Area of the Arch is Crowded
Makes more Sense to Replace with Implant
Tooth prevents Access to another Tooth
Note – it May be to Expensive to get the Tooth Extracted
………………………………………………………………………………………………………………………..
Only Root Left
It may be that you have some teeth that started breaking down years ago, and there is nothing left of the crown of the teeth. Then the roots started erupting more and more and have been eroded away as they moved, and there is little left showing in the mouth except just a part of the root, which may just be the root tip. This is the simplest extraction ever, just requiring grabbing the piece of root with some forceps and giving a little tug. It will not need much in terms of anesthesia, as there is little connection left with the bone – it is only the soft tissue that would hurt a bit. These extractions are easy for the dentist and he/she should not charge much for the procedure – on the other hand if your insurance covers it, the dentist will get paid the same as for a more difficult extraction and that is good for them.
Tooth Riddled with Decay
If the tooth needs extraction because it is riddled with decay, which has undermined much of the crown of the tooth, either involving the pulp chamber or not, and the restoration process seems to be challenging at best and impossible at worst, extraction may be a reasonable option. It is up to the dentist to decide what the odds are of success of rebuilding the tooth, but if he thinks the odds are 50% the patient may decide it is not worth the risk of wasting their money. Saving the tooth could involve crown lengthening to establish margins in solid tooth structure below the original level of the gingiva, then a root canal, then a post and core buildup, then the crown, which adds up to a lot of money. And, at any point in the procedure it may be discovered that there is a crack in the remaining tooth structure which goes farther gingivally down the root, meaning the tooth is doomed anyway.
Decay in Furcation between Roots
If there is decay in the furcation of a tooth, where multiple roots come together – which can only happen if the patient has significant gingival and bone recession – this may be virtually impossible to restore. The access to this area with a bur to remove the decay and establish the appropriate form to retain a restorative material is generally challenging to say the least. And the decay will have encroached significantly on the floor of the pulp chamber at this point, perhaps necessitating root canal therapy, but leaving an area where it is difficult to establish an adequate seal. Most dentists will recommend extraction of the tooth in this situation, electing not to do “heroic” work.
Periodontal Reasons
Some teeth are extracted because of periodontal reasons. If the tooth has lot so much bone support, and gingival recession has happened to the point where much of the root is exposed, suggesting more likely root decay, and the tooth isn’t really supported by the bone anymore so it moves around easily, it is no longer a useful tooth and should be extracted. For most of the world edentulousness (having no teeth) is caused by periodontal disease – and the periodontal disease was allowed to run amok because of poor attention, home care and little professional help. Most denture wearers became such as a result of periodontal disease, with methamphetamine addition in the U.S. catching up fast for the younger person.
Vertical Fracture into Root
Vertical fracture into the root is also a common reason for extraction, even for someone who can afford “heroic” or expensive procedures. There is basically no chance of saving a tooth with such a fracture. The root canal therapy can be done, but there will also be a leak into the canal system through this crack, with attendant recurring infection into the bone at the apex.
Tooth not Needed
It may be that a tooth is extracted just because it is not needed. This may be due to the opposing tooth having already been extracted. If you have an upper second molar (with no wisdom tooth behind it) but there is no lower second molar opposing it, and there is no plan to replace it with an implant, then extraction would be an option. While we would LIKE to keep the second molars for better chewing function, they are not necessary. In fact, if you have ALL of your teeth replaced with implants, generally the appliance that is attached to these implants will NOT extend back farther than the location of the first molar. The situation is a little more obvious if we are talking about an unopposed third molar (wisdom tooth). Of course, if you have an EXTRA tooth (supernumerary tooth) which has not erupted into occlusion with any opposing tooth, it is useless and can be removed at any time, mostly just to make it easier to clean the adjacent teeth. I had a FOURTH MOLAR on the upper left side which started erupting in my 50s! Certainly, it was of no FUNCTIONAL use, but I kept it and let it grow in for 20 years. WHY did I do this? Well – I figured that if the third molar is a “wisdom tooth”, a fourth molar had to be smarter than that, and I just wasn’t willing to part with any smarts I could get! Well – now it, AND the third molar are both gone, so that I can have the area cared for more thoroughly by periodontal therapy – but think of how good this website would be if they were both still there!
Too Expensive to Restore Tooth
Maybe it’s simply too expensive to keep a tooth in place, and extraction is the only viable choice. Considering it may cost thousands of dollars to keep a tooth, spending a few hundred to get it out seems like a reasonable choice. Unfortunately, the fact that there is a missing tooth will inevitably lead to more problems down the road, but extraction was the best solution for now. Hopefully the financial situation will be better later to deal with the changes in the mouth that will likely ensue with the missing tooth. Of course, if it is a front tooth, particularly on the top, SOME kind of replacement is desirable, and the least expensive of these, a “flipper”, may still work within the budget. For the consequences of missing teeth visit Chapters III.9 and V.13.
Tooth is Impacted
Impaction is another reason for extraction. Here we are typically talking about third molars, the ones that are supposed to come in during your late teens or early twenties. Sometimes third molars are positioned completely wrong for eruption. They may be pointed TOWARD the second molars, instead of parallel to it, basically hitting the second molar at an angle. IF the point of contact is closer to the point where the enamel of the second molar ends and the root starts, the pressure of the third molar will often cause resorption of the tooth structure on the back side of the second molar. This may or may not involve decay, but it can either way penetrate until it exposes the pulp of the second molar and root canal therapy is needed. The problem here is that after the RCT the back side of the tooth where the erosion took place needs to be patched up, and that cannot be done without removing the third molar anyway. So, best to get it done before the damage is irreversible to the second molar. Also – the third molar can be positioned so horizontally that it is completely buried within the bone while approaching the root of the second molar under the bone level. While a tooth CAN potentially be left in this position for some period of time, this FULL BONEY IMPACTED tooth will likely be removed eventually. The process is more difficult, as you might imagine, requiring removal of the bone over the tooth before lifting it out. More about this when discussing difficulties of extractions below.
Tooth is Crowded into Arch
Crowding is the most common reason for removal of teeth – and this is actually another example of a tooth that is not needed. In my teens I had a canine erupt high up above the level where it should have, up on the outside of the ridge, because there was no room for it to come in normally. The canine is often the last tooth to erupt in that area, and my first and second premolars were already in. The canine is a very important tooth, providing what we have discussed before as “canine guidance”, which forces the back teeth and front teeth to separate when you shift your jaw from side-to-side or front-to-back. So, I had my first premolar extracted simply to make room for the canine to erupt. Of course the canine now had to be guided into place orthodontically. But it is common when a child goes into braces for the dentist to recommend extraction of several teeth to keep the arch form natural and not crowded.
Space needed more for Implant
Another situation that sometimes occurs is when there is a space that you would like to fill using an implant, but an adjacent tooth is leaning into that space, making the placement of the implant problematic. In this case it MAY be possible or desired to tip the offending tooth back where it belongs using an orthodontic procedure, but it also may be far easier to simply extract it if the implant-supported prosthesis can fill the somewhat larger space safely. In this case there are choices to be made that depend on the exact situation, but extraction is a possibility.
Need Access to another Tooth
I’ve already mentioned the possibility that one tooth can sometimes prevent access to another, either for allowing efficient and complete periodontal instrumentation, simply to improve the ease of home care, or because one tooth is blocking access for the restoration of another, more necessary tooth.
Many situations may prevail that would suggest extraction of a tooth, and we’ve just discussed many, and there are many more that continue to show up on an individual basis.
Expensive of Extraction
One of the things that MAY determine the choice of extraction or not is the difficulty of the extraction, which will be the subject of the next section.
Factors Determining the Difficulty of a Dental Extraction
As we’ve seen, there are situations where the extraction of a tooth, or what is left of it, is very simple.
I just had a memory of the time I went to visit my grandmother toward the end of her life. She was still living alone, and when I got there on that occasion I found on the table next to her favorite chair, two teeth that SHE had extracted! I was not a dentist at the time, but knowing what I know now, it is clear that the teeth were periodontally involved and really “loose”, or mobile because of little or no bone support, and she just rocked them back and forth until they came out. This was probably with a minimum of discomfort for her as the bone was not involved. Now THAT is a simple extraction.
Basic Method
But for moderately difficult extractions, it is not likely that you will do that at home. When a tooth is extracted that is still firmly held in the bone, the the periodontal ligaments are still well connected to the surface of the root, it takes more than a casual rocking back and forth. The dentist will need to hold the crown of the tooth FIRMLY with one of many different forms of extraction forceps (each designed for a particular tooth or situation) and LUXATE the tooth. That means tipping it forcefully toward the facial and lingual sides, toward the cheeks and tongue, forcing the BONE TO EXPAND. It is the expansion of the bone that allows more room for the tooth to move so the periodontal ligaments will tear. Ideally, after rocking the tooth back and forth a number of times, firmly but slowly, the tooth can be somewhat rotated so more ligaments tear, and eventually the rocking becomes easier and easier and the tooth just gives up and slides out.

There are times when the bone around the teeth has become more dense than usual, or the roots are particularly LONG into the bone. In these situations the expansion of the bone requires more strength and patience than the dentist may have available to him/her. In this case the crown of the tooth may break under the excessive load.
Tooth Breaks during Extraction or Was Broken Before
IF the reason for the extraction is that the crown of the tooth is badly broken down, then you can imagine there will be little to grab onto to effect this expansion of the bone. In this case, the dentist will be VERY careful for the first few rocking movements, hoping that the tooth stays intact while there is SOME expansion of the bone achieved. The dentist may even use a chisel-like instrument to push down into the space between the tooth and the bone to attempt to PRY the tooth from side to side, expanding the bone without putting so much pressure on weaker parts of the crown. BUT – at some point the crown will break and there will be little or nothing left for the forceps to hold on to. At this point the dentist will have to use various shapes and sizes of these chisel-like instruments, called elevators, to pry up one part of the tooth or another. It is possible that if the breakage is near the furcation of the tooth, where the roots come together, that if there are multiple roots, the tooth structure will break between them. In this case the dentist will pry out each root individually. The dentist may have to actually cut the tooth between the roots so that they CAN be extracted separately.
I know none of this sound pleasant, and it is not particularly to the dentist either, but probably you’d rather just let them do their job without knowing the details ….
Challenging Situations
Bulbous Roots
Ankylosis
Curved Roots
Roots into Sinus
Roots near Nerve
Impaction
……………………………………………………………………………………………………………………….
Really difficult extractions are caused by certain deviations from ideal.
Bulbous Roots
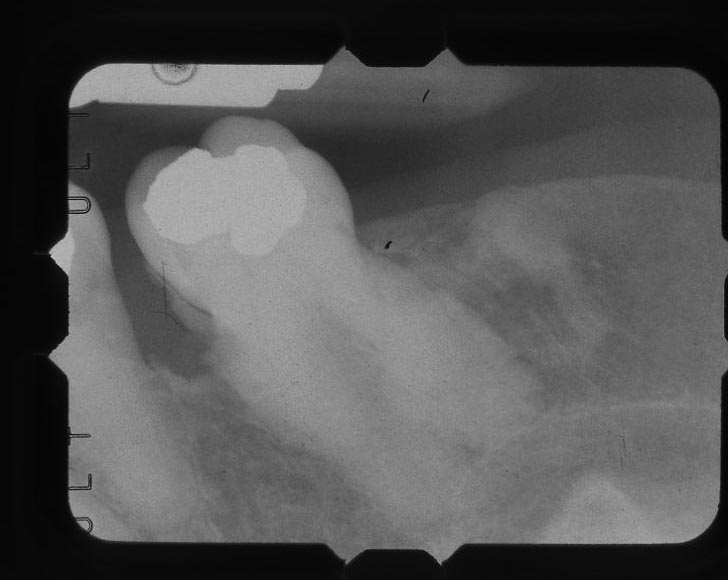
If there is only one root for the tooth, or if there are multiple roots, one thing that is sometimes observed is that the cementum of the root has grown thicker than it is supposed to. This is called hypercementosis – too much growth of cementum. It is supposed to be just a thin layer, but for some reason (I don’t know) it can expand greatly. The X-ray below shows such a case of BULBOUS ROOTS. Can you imagine using the technique described above to get that tooth out? The size of the root will NEVER pass through the hole in the bone that surrounds the upper part of the tooth. To do this extraction it would require removing a lot of bone first, so that the bulgy area could pass through.
Ankylosis
Another situation which requires special attention is when the periodontal ligaments that support the tooth in the bone are GONE – and the tooth is firmly locked into the bone. This is called ankylosis. The tooth is, effectively, part of the bone – is a continuation of the growth of the bone. The good news is that it is unusual to NEED to extract such a tooth – often they are not even erupted. In fact, the eruption process requires the presence of the periodontal ligaments. BUT, if the situation is that an implant needed to be placed in this area, the ankylosed tooth would have to be removed first. Definitely a job for an experiences surgeon!
Curved Roots

Another situation that makes extraction difficult is when there is a multirooted tooth and the roots curve toward each other at the apices – effectively HOLDING ONTO the bone, as if the roots are hugging the bone within curved arms. In this case it is clear that the tooth is NOT going to simply come out with luxation – and the dentist will quickly cut the tooth into pieces so that each root can be extracted separately. It still may be a difficult process, if the curvatures require the roots to interfere with each other as they are extracted – but an experienced oral surgeon or dentist can manage this situation comfortably in most instances. It may also be that bone is trapped between roots of adjacent teeth, as the above picture illustrates.
Roots into Sinus
Another difficult extraction is one where the apices of the roots lie within the sinus – that void above the upper teeth that sometimes gets infected. The sinus chamber is lined by a membrane, which must not be breached, but the amount of bone between the sinus and the upper molars and premolars is quite variable. Sometimes the amount of bone below the sinus is very THIN! If a dentist is not sufficiently careful in this case, it is possible that the floor of the sinus will break out as force is placed on any tooth passing through this thin layer of bone. That is something that must be avoided at all costs, and will require an experienced surgeon to repair. The good news is that the X-ray easily shows when there is any risk for this to happen, and I, personally, always referred such extractions to the oral surgeon.
Roots near Nerve
Another possibility that is cause for some concern is when the roots of the tooth are near a large nerve. This is possibly the case for the lower teeth, where there is a large nerve running in a canal through the jaw bone along each side. The canal which conducts the nerve is often visible on the X-ray, so if there is any possible problem it is generally known from the start. Normally, a typical extraction by luxation would be done comfortably no matter what the nearness to the root is, but if the root breaks and leaves a ROOT TIP at the bottom of the socket, it is necessary to pry the root tip back out using ROOT PICKS. If the dentist is working near the root apex with sharp instruments, and the bone at that point is very THIN between there and the nerve, there is reason for considerable caution. This represents a potentially hazardous situation, but one that dentists are trained to be aware of.
Impaction
This is often the case when third molars just refuse to erupt – they are lying in the bone horizontally. There are situations where the tooth is partially coming out of the bone, and also where the tooth is completely covered with bone, referred to as a “full boney impaction”. These represent more of a challenge, especially when lying on the nerve – but are regularly managed by oral surgeons.

Dental Extractions: Methods
A lot has already been said about the general approach to extraction by luxation and some of the complications that can occur and what can be done about that.
To summarize, there are four basic levels of extraction technique:
- Removing the tooth by luxation, rocking back and forth until it loosens enough to slide out. This works well for any tooth that is single rooted and the root is conical in shape, or multiple roots and the roots are not too curved. More discussion was given earlier.
- Sectioning the tooth into parts and extracting each part separately. This is generally not required for single root teeth, but for multiple roots that are curved it often will be required. The dentist will drill down into the socket, often after the crown of the tooth has already broken off, and cut through the tooth between the roots. The dentist must be careful to avoid as much as possible cutting into the bone and only cut the tooth, but the bone will typically fill back in anyway. Sectioning the tooth is a pretty common procedure which many dentists are comfortable with, but if it is thought to be necessary, most dentists will refer to an oral surgeon for that extraction.
- Bone removal over or around tooth, is sometimes required. This would only be done by a dentist who has more than the usual training in oral surgery, or by an oral surgeon. As we’ve discussed, it could be a bony impaction case, or it could be bulbous roots, or even where there is a thin sinus floor. In the latter case, to reduce the stress to the bone on the floor of the sinus, the dentist will not want to luxate the tooth in order to remove it – so it will be more common to section the tooth immediately, and then cut bone on the alveolar ridge surrounding the root of the tooth, rather than expanding it or prying against it. Any force that tends to fracture the floor of the sinus is to be steadfastly avoided.
- Removal of tooth by exposing the bone covering it. In this case, whether it is that the tooth is entirely embedded in bone, or ankylosed, or angled forward toward another tooth so it cannot come out in the direction it is pointed, the dentist will commonly pull back the gingival tissue surrounding the tooth, and additional tissue over the palate or alveolar ridge, so as to expose the entire bone structure over the tooth that needs extraction. The dentist will use a scalpel to cut the tissue around the teeth, or make an incision along the ridge where no teeth protrude, and gently lift the tissue away from the bone. This FLAP is STILL CONNECTED to the rest of the tissue over the palate or into the facial and lingual surfaces of the ridge, because it is through that connection that the BLOOD SUPPLY for the flap is obtained. When the flap is sutured back into place after the extraction is done, it will only heal if the blood supply is good – and every dentist knows to make sure it is.
Recovery from Dental Extractions
Routine
Many people have tales they tell about when they were kids and had all of their wisdom teeth extracted and their face swelled up like a pumpkin for the next week. This is NOT always the situation, of course.
The recovery process has a lot to do with the amount of trauma that is incurred in the region of the extraction. The application of great force is traumatic, and the bone and tissues will not recover very gracefully perhaps. If the dentist decides to section a tooth and remove it in parts, it can be far less traumatic. But, if the tooth is fully impacted under the bone, there will be a surgical trauma to removing parts of the bone that may engender some swelling afterward.
A simple extraction requires little recovery period. Once the tooth is out and the socket is clear, as long as a BLOOD CLOT forms within the socket, the area will heal comfortably. The dentist will often scrape the sides of the tooth socket after removal to stimulate the flow of blood, then supply the patient with a piece of gauze so that the clot will form and be kept in place for a few hours. If the clot is dislodged and the socket does not bleed again, there is the possibility of a DRY SOCKET – this can be painful, as it is an area of exposed and sensitive bone, which has plenty of nerves. The dentist will then have to chemically restimulate the flow of blood and the formation of a new clot. We usually council patients NOT to use drinking straws or do anything after a simple extraction that would generate vacuum in the mouth, thinking that dislodgment of the clot could occur.
Bleeding
Excessive bleeding is also something to watch for. Normally a person’s clotting mechanism is just fine for the formation of an appropriate clot and the stoppage of any additional bleeding. Sometimes people THINK that there is too much bleeding when there is actually very little – a little blood in the mouth can look like a LOT. On the other hand, if the person has a compromised clotting mechanism, perhaps because they are taking blood thinners, that is another matter. In this case the dentist would normally consult with the prescribing physician and have the patient either stop the blood thinners for a few days, or shift to another medication which is more short-acting.
Suturing
Also, there are times when leaving the socket open less advisable. The vast majority of extractions heal very well with just some gauze and some time. But, if the dentist wants the healing process to proceed more quickly or controllably, or perhaps more comfortably, they can suture the socket closed after the extraction. Of course they cannot close the entire socket because there was not enough tissue there with the tooth in place to pull it that much farther. But, there are gel-like materials that can be sutured into the socket to provide a scaffold for the formation of a clot, and these materials are sutured in. The gel will resorb as the clot forms, and as more bone forms to fill the socket in, and perhaps the dentist will use resorbable suture thread as well so another visit is not required to remove the sutures. Of course, there is additional cost to this procedure, and it is not necessarily a gain in comfort in many instances.
Bone Grafting Situations
On the other hand, there are times where after the extraction the dentist will want to encourage the growth of more bone to fill the socket more completely and quickly. This is most usual for a case where the intention will be to replace the extracted tooth with an implant. Since the implant is supported by bone, it would be best to have more solid bone. This is achieved by placing BONE GRAFT material into the socket, with a membrane covering it, and then closing the area with sutures. This provides the best possible geometry for the new bone so the implant is likely to be successful.
Bone grafting is also sometimes done when the tooth is extracted and then an implant is immediately placed, with bone graft material around it. The implant in this case is “buried”, not showing on the surface of the mouth (it will be uncovered later). The implant and graft are all covered up with a membrane and the site sutured as above.
So there are a variety of different procedures that involve extraction, and the extraction itself may not be the only procedure done. This will determine the way the extraction site is managed after the extraction – ranging from simply letting it heal, to advancing the healing process as much as possible with additional procedures.
In any case, the recovery from extractions, whether simple or complex, does not have to involve much discomfort or inconvenience. The greatest inconvenience for most people is that the INDENTATION from the socket after it has been closed over with more tissue growth, will tend to collect food particles for a while.
Bottom Line for Dental Extractions
While having a tooth extracted is never a pleasant prospect, there are times when it involves very little trauma or discomfort.
On the other hand, of course, there are situations where the difficulty of and recovery from the extraction is more unpleasant.
We have seen many situations in which extractions are recommended.
We have seen the basic and more advanced techniques for doing these extactions.
And, we have seen what the recovery process entails, depending on the circumstances of the extraction and the techniques utilized.
It is important to realize that the CONSEQUENCES of an extraction are another consideration. In Chapter III.9 we discussed missing teeth, and in Chapter V.13 we will discuss the replacement of teeth that are missing for whatever reason, but often due to their having been extracted.